Joe Moore and Anne Philippi (New Health Club) are hosts of the PS25 Morning Show! This one features Cesar Marin, AnneClaire Stapleton, Dennis Walker, Jonathan Sabbagh, Tom Feegel and Philip Graf von Drechsel!
And thats a wrap for PS25!!
Joe Moore and Anne Philippi (New Health Club) are hosts of the PS25 Morning Show! This one features Cesar Marin, AnneClaire Stapleton, Dennis Walker, Jonathan Sabbagh, Tom Feegel and Philip Graf von Drechsel!
And thats a wrap for PS25!!
Joe Moore and Anne Philippi (New Health Club) are hosts of the PS25 Morning Show! This one features Dee Dee Goldpaugh, LCSW and Tommaso Barba, PhDC!
We talk about all things Sex and Psychedelics!
In this episode of Psychedelics Today, kicking of Psychedelic Science 2025 week in Denver, we sit down with Jonathan Dicksinson, Chief Executive Officer, and Trevor Millar, Chief Operations Officer of Ambio Life Sciences – one of the world’s leading ibogaine clinics – to explore the potential of ibogaine for addiction, neuroregeneration, and how ethics, honoring experience, and sustainability will be key to delivering ibogaine at scale.
Trevor shares his early work supporting marginalized populations in Vancouver’s Downtown Eastside, which led to the founding of Liberty Root, one of Canada’s first ibogaine clinics. Jonathan reflects on his apprenticeship in Mexican clinics, years of international advocacy with the Global Ibogaine Therapy Alliance, and drafting the first set of clinical guidelines for ibogaine detoxification. Together with paramedic and ibogaine safety protocols expert Jose Inzunza, they co-founded Ambio in Tijuana in 2021.
They discuss:
They also make a compelling case that Ambio is already modeling what the future of psychedelic care should look like – not a single drug in a sterile clinical setting, but a comprehensive, integrated protocol combining preparation, medical oversight, and deep integration. “Start with the end in mind,” Trevor urges – Ambio isn’t just part of the movement; it’s the blueprint for how ibogaine could be delivered worldwide.
Links:
Aspen Psychedelic Symposium 2024 – Hosted by Kevin Franciotti
This panel explores the healing power of Ibogaine, a powerful plant medicine used for addiction recovery and spiritual growth. Moderator Kevin Franciotti leads a thoughtful conversation with Talia Eisenberg, Tom Feegel, and Dr. Lola “Dr. O” Hoba. Together, they cover personal healing, clinical safety, and the need to protect traditional knowledge.
Talia Eisenberg shares how a single Ibogaine experience helped her break free from opioid addiction. That moment inspired her to co-found BEOND Ibogaine, a treatment center in Cancun. Tom Feegel, her husband and co-founder, explains how his own recovery journey led him to help build a safe, medical space for others to heal. Their stories show how Ibogaine can open a path to deep personal transformation.
Dr. Lola Hoba blends Western science with her Yoruba heritage. She explains that Ibogaine works across several brain systems, reducing cravings and supporting lasting recovery. Unlike other psychedelics, it also carries medical risks. For this reason, Dr. Hoba urges proper medical screening and trained facilitation. She adds that spiritual respect is just as important as science.
At BEOND, safety comes first. Patients go through detailed screening and are supported by ICU-trained doctors and nurses. Each experience is closely monitored, ensuring both physical and emotional care. This approach combines hospital-level safety with the warmth of a retreat. According to Tom, healing begins with love—not just medicine.
Iboga comes from Central Africa and grows slowly. Unfortunately, growing demand has led to poaching. To give back, BEOND partners with Blessings of the Forest, a nonprofit in Gabon that protects Indigenous access and wild plant populations. As Ibogaine use grows, the panel stresses the importance of honoring the cultures that have carried this wisdom for generations.
Ibogaine shows strong potential for treating addiction, PTSD, and depression. However, U.S. access remains limited due to medical risks and legal hurdles. Even so, hope is growing. The panel calls for responsible expansion, better aftercare, and policies that prioritize both science and justice.
Thanks to Aspen Public Radio, Aspen Psychedelic Resource Center, Healing Advocacy Fund and Aspen Psychedelic Symposium for allowing us to share this podcast.
A full agenda from the symposium can be found here.
In this riveting and deeply personal conversation, moderator Jim Harris is joined by three pioneers at the intersection of neuroscience, psychedelics, and disability: Dr. Rachel Zoeller (Doctor of Physical Therapy and spinal cord injury survivor), Dr. David McMillan (Assistant Professor of Neurological Surgery at the University of Miami), and Dr. Manesh Girn (neuroscientist and postdoctoral researcher with Robin Carhart-Harris at UCSF). Together, they explore how psychedelics may do far more than treat depression or catalyze mystical experiences—they may also support healing and regeneration in the nervous system.
The discussion opens with an acknowledgment that our cultural understanding of psychedelics has mostly focused on their psychological and spiritual effects. But as these experts reveal, the somatic potential of psychedelics is vast and understudied. They delve into promising areas like central and peripheral neuroplasticity, the anti-inflammatory effects of psychedelics, and how these mechanisms might play a role in healing from spinal cord injuries or paralysis.
Dr. Girn breaks down the science behind psilocybin’s interaction with 5-HT2A serotonin receptors, not only in the brain but also in the spinal cord. These receptors, when activated, may increase neuronal excitability and even help restore lost signaling in damaged motor pathways. He suggests that psychedelics could reopen “critical periods” for neuroplasticity—windows of opportunity for the nervous system to rewire and heal.
Rachel Zoeller shares her powerful lived experience as both a physical therapist and a spinal cord injury patient. Her story brings the science to life, particularly her observation that psychedelic experiences help her reconnect to parts of her body affected by paralysis. Psychedelics, she suggests, have allowed her to rebuild mind-body communication and foster compassion toward her own physical limitations. She also underscores the need for patients to cultivate body awareness, meditation, and breathwork as essential tools for safe and effective psychedelic use.
Dr. McMillan, who leads outreach at the Miami Project to Cure Paralysis, provides a clinical and safety-oriented perspective. While optimistic about the potential, he urges caution—especially with individuals who have high-level spinal cord injuries and are vulnerable to serious complications like autonomic dysreflexia. He stresses that before we can bring these treatments into clinical settings, we must carefully assess physiological risk, develop precise pharmacological protocols, and prioritize patient safety.
The panel also addresses cultural and spiritual interpretations of spasticity. Drawing on both shamanic and somatic perspectives, they propose that these involuntary muscle contractions could be reinterpreted not as dysfunction, but as potential portals for healing, integration, or neurological feedback. The idea that such spasms might help the brain remap muscle groups is discussed as a provocative and hopeful reframe.
The conversation wraps with a call to action: to bring together indigenous wisdom, embodied knowledge, rigorous science, and community storytelling in order to chart a new frontier in psychedelic medicine—one that does not leave the disabled community behind. As McMillan puts it, “There’s a lesson to psychedelia from paralysis.” It’s a reminder that neuropharmacology must consider not just molecules and mechanisms, but people and possibilities.
Whether you’re a clinician, researcher, patient, or curious explorer, this panel is a moving and illuminating look at how psychedelics could transform not only minds—but bodies.
Thanks to Aspen Public Radio, Aspen Psychedelic Resource Center, Healing Advocacy Fund and Aspen Psychedelic Symposium for allowing us to share this podcast.
A full agenda from the symposium can be found here.
In this episode, Kyle Buller speaks with Kayse Geheret, founder of Microdosing for Healing and instructor for Psychedelics Today’s Vital program. They explore what it means to be a modern guide in the world of psychedelics. Kayse shares how microdosing has become a key entry point for many and highlights the importance of training, community, and personal growth.
They discuss how not all psychedelic work involves facilitation. Some guides support through integration, education, or community organizing. The conversation covers what makes a great guide—qualities like groundedness, empathy, curiosity, and the ability to hold space. They also talk about the growing need for psychedelic-literate professionals in all fields, not just therapy.
Kayse and Kyle reflect on the importance of finding the right training—whether for coaching, integration, or peer support. With more people entering the space, education and connection are more important than ever.
Whether you’re curious about microdosing, thinking of becoming a guide, or simply want to better support your community, this episode offers valuable insight.
🎧 Learn more at microdosingforhealing.com
🌱 Discover Vital at vitalpsychedelictraining.com
In this episode of Psychedelics Today, Kyle Buller is joined by Dr. Hannah McLane, founder of the SoundMind Center and SoundMind Institute. They dive deep into the evolving psychedelic landscape—touching on policy developments in New Jersey, Massachusetts, Pennsylvania, and beyond. Dr. McLane shares her experience testifying in support of psilocybin legislation and discusses the medical frameworks being explored, particularly in contrast to Oregon and Colorado’s models.
The conversation also explores the essential qualities of effective psychedelic facilitators, emphasizing the importance of self-awareness, lifelong learning, and doing personal inner work. Dr. McLane offers insights into the challenges of entrepreneurship in the psychedelic space, balancing mission-driven work with sustainability, and how neurodiversity and trauma have shaped her approach.
Toward the end, the conversation takes a playful and heartfelt turn, reflecting on parenting, the power of curiosity, and the need for more community-centered, human-first spaces for integration and healing. This is a rich, honest, and inspiring dialogue that bridges the personal and political, the clinical and ceremonial, and the visionary future of psychedelics.
https://www.hannahmclanemd.com/
As society becomes more virtual and disconnected, many of us are looking for new ways to touch, feel, and connect. What is Kama Flight, and how can it be used with psychedelics?
In this episode, Joe interviews Jeremy Falk: certified instructor and training program developer for Kama Flight; and Dr. David Rabin, MD, Ph.D.: board-certified psychiatrist and neuroscientist, co-founder & chief Medical Officer at Apollo Neuroscience, and advisor to the non-profit, Kama Flight Foundation.
Kama Flight is a wellness modality for partners, inspired by the movements of Watsu therapy, Thai massage, 5Rhythms, tango, improv dance, and Acroyoga. At the heart of it is the dynamic between the two people engaged in the dance (the ‘base’ and the ‘voyager’), which touches on collaboration, leadership, receptivity, strength, surrender, and most importantly, trust. The communication and instant feedback shared between the partners mixed with the healing energy of the somatic movements results in moving stuck energy out of their bodies while also making them more comfortable with touch, agency, and consent – which could be extremely beneficial toward preparing for a psychedelic experience.
They talk about:
and more!
In addition to running retreats, Kama Flight is teaching their craft as well, and just finished their first training. They’ve launched an at-home course, and have upcoming workshops in Austin, New York City, and Miami, with the next taking place this Saturday, Jan. 18, in Mill Valley, CA. Use code KAMAFLIGHTPT for 15% off!
Gnar Country: Growing Old, Staying Rad, by Steven Kotler
Hhs.gov: U.S. Surgeon General Issues New Advisory on Link Between Alcohol and Cancer Risk
Kama Flight retreat: Jan. 30 – Feb. 2, at Casa Maya Kaan, Tulum, Mexico
Kama Flight’s other upcoming classes
Kama Flight class: Jan. 18 at The Portal, Mill Valley, CA (use code KAMAFLIGHTPT for 15% off)
*Amazon links are affiliate links, meaning that Psychedelics Today will receive a percentage of the sale
What is RSO? What is THC-A? Do sativa and indica really mean what we think? How much do we really know about cannabis?
In this episode, Joe interviews Angie Roullier: longtime veteran of the cannabis industry and author of the book, Pot for the People: The Plant, the People, and the Shop Policies of Cannabis.
Diagnosed with the neurological disorder, Charcot-Marie-Tooth (CMT), Roullier tells the story of how cannabis replaced all her medications, which led to a personal journey and career centered on cannabis education. She talks about the challenges patients face in today’s rapidly evolving cannabis markets, misconceptions surrounding cannabis, the ignorance of many budtenders, and how not knowing enough can lead to an underwhelming high. She discusses how she educated people in shops and how her book was written to teach people how to ask the right questions to not only ensure a safe and effective experience, but to also give them the experience they’re looking for.
She talks about:
and more!
Mayoclinic.org: Charcot-Marie-Tooth disease
Hereditary Neuropathy Foundation
Leafly.com: What is Rick Simpson Oil? Your complete guide to RSO
Burningdaily.com: Is THCA Legal in South Carolina? Understanding the Legal Landscape
YouTube: Grandmas Smoking Weed for the First Time (likely the video Joe is talking about)
Psychedelics are going mainstream, but society’s views on addiction and recovery models are still behind. Is the recovery community ready for psychedelics?
In this episode, Joe interviews Dan Ronken: licensed professional counselor and addiction counselor with a private practice in Boulder, CO, called Inclusion Recovery, and lead trainer and facilitator for the Integrative Psychiatry Institute (IPI).
He tells his story of going from a sponsored BMX racer to three stints in rehab before the age of 14, and what he’s learned from his experiences in recovery over the years: that there is a wide range of what ‘in recovery’ actually means, that abstinence-only and 12-step models don’t work for many, that connection and community – and consistency in both – are enormous parts of what actually leads to overcoming an addiction, and more. As recovery communities cautiously begin to talk about psychedelics, he highlights the importance of nuance in understanding addiction, the need for open-mindedness toward new therapeutic approaches, and the need for diverse support networks that welcome discussions around psychedelics.
He talks about:
and more!
Nature.com: Ketamine can reduce harmful drinking by pharmacologically rewriting drinking memories
Alcoholics Anonymous: The Big Book
Lucid.news: Bill Wilson, LSD and the Secret Psychedelic History of Alcoholics Anonymous
YouTube: Bill W. (2012 documentary)
The Rose Of Paracelsus: On Secrets & Sacraments, by William Leonard Pickard
*Amazon links are affiliate links, meaning that Psychedelics Today will receive a percentage of the sale
Faced with health challenges that traditional treatments often fail to remedy, veterans are increasingly turning to psychedelics for help. Their stories of trauma and healing help humanize their experiences, reduce stigma, and foster essential conversations that broaden acceptance and understanding of how psychedelics can support them.
While over 7,000 U.S. service members have died in combat since 9/11, more than 30,000 veterans and active-duty soldiers have taken their own lives during the same period. Some estimates suggest this number could be significantly higher, reaching upwards of 150,000. This staggering statistic highlights a mental health crisis, one in which veterans face PTSD, depression, chronic pain, insomnia, and other challenges at alarming rates. Many veterans feel abandoned by traditional therapies that often provide only temporary relief.
With increased advocacy and a surge in scientific support, psychedelic-assisted treatments have emerged as a promising pathway for veterans seeking more comprehensive recovery from trauma.

After leaving combat, former Army Ranger Jesse Gould struggled with severe PTSD. He left his career as an investment banker, sold his belongings, and journeyed around the world in an attempt to find a new way forward.
After an ayahuasca retreat in Peru, Gould says he – finally – found relief from his PTSD symptoms. Invigorated by his experience and the relief he found in plant medicine, Gould founded Heroic Hearts Project, a nonprofit dedicated to supporting veterans and their families in overcoming the impacts of PTSD and military trauma.
“I was at my lowest point, feeling disconnected and hopeless,” Gould told Psychedelics Today. “As my own pain began to lift, I knew I couldn’t keep this journey to myself.”
Heroic Hearts empowers veterans and their loved ones through transformative retreats and encourages them to take control of their healing. The organization fosters community and provides support for veterans as they undertake the challenging work of processing trauma and reclaiming peace, Gould says. It builds ‘psychedelic literacy’ through education on preparation, integration, and safe practices for maximizing benefits.
“When veterans have these big psychedelic experiences during a retreat, no matter what, they will have lasting changes,” Gould explains. “They gain new perspectives on how they view themselves and the world.”
Ensuring veterans have not only have access to a community, but that they’re armed with a strong foundation of psychedelic therapy, integration, and risk reduction is crucial to ensuring their relief is durable, says author and educator Matt Zemon MSc.
A new book, The Veteran’s Guide to Psychedelics, written by Zemon in collaboration with Heroic Hearts and clinically reviewed by Ken Weingardt, PhD, was recently published to help bridge this critical knowledge gap. Gould and Zemon kicked off the project after Gould noticed the lack of comprehensive publications tailored for veterans exploring psychedelics.
The clinically reviewed book was designed to equip veterans with knowledge of safe, responsible, and therapeutic psychedelic use, offering insights into a new frontier of mental health care that emphasizes key principles veterans need to understand when exploring psychedelic options responsibly.

Dr. Robert “Bob” Koffman, a retired Navy Captain and psychiatrist, emphasizes the significant gap in addressing the trauma many veterans face.
“For years, like most clinicians, I relied on conventional treatments… but despite our best efforts, the standard approaches often fell short,” he explains.
This realization led him to explore psychedelic-assisted treatments, which he views as potentially transformative for veteran mental health care.
With nearly 40 years in military medicine, including combat experience and public health expertise, Koffman has seen firsthand the limitations of traditional approaches. He believes that psychedelics – particularly those promoting neuroplasticity – can address trauma in ways conventional methods cannot. According to him, these therapies may “not just heal hidden wounds, but by mending the accompanying soul wounds, and save countless families.”
Koffman emphasizes the importance of health literacy for veterans: “It’s about knowing what questions to ask, recognizing the risks, and understanding the potential benefits.”
For him, informed preparation and responsible use are essential for veterans to move from crisis to genuine transformation and long-term wellness.

According to Zemon, openly sharing stories is a powerful force for fostering understanding and encouraging other vets to explore new avenues of healing. Many veterans who have turned to psychedelics describe their experiences as life-changing, inspiring fellow veterans to consider new possibilities for their own recovery.
Tom Satterly, Delta Force veteran and co-founder of All Secure Foundation, says psychedelics allowed him to confront trauma in ways conventional therapies could not.
“These treatments have allowed me to break through pain that no other method could touch,” Satterly said.
Steve Keefer, a veteran of the 2nd Ranger Battalion, says his perspective evolved through sacred ceremonies supported by community. “I viewed life as a series of battles, but this attitude strained relationships and led to negativity. Through healing ceremonies, I’ve found fulfillment, peace, and healthier relationships. I’m more in service to others now than I ever was in uniform.”

“Veterans need a clear understanding of the risks, as well as a strong foundation in preparation, set, setting, and integration – each essential for veterans who choose this path to navigate it successfully,” Zemon said.
Zemon advocates for a proactive approach, encouraging veterans to balance both potential benefits and risks in considering psychedelic-assisted healing.
“While psychedelics offer new possibilities for healing, they must be approached with caution and preparation,” Koffman adds.
The conversation around psychedelics in veteran mental health is evolving, and at its core is an urgent need for psychedelic literacy and supportive resources. Bridging this knowledge gap with science, safety, and empathy equips veterans with the guidance they need. By understanding the critical elements of psychedelic therapy and the organizations that facilitate access, veterans can embark on a healing journey that addresses trauma holistically and cultivates renewed hope.
With so much attention being placed on the psychedelic experience itself, too many people are getting stuck in patterns of chasing the experience without making space for integration.
In this episode, Kyle interviews Lana Pribic, M.Sc: host of the Modern Psychedelics podcast, certified professional life coach, and founder of Kanna Wellness.
She talks about her early days of rave culture and MDMA, to exploring other substances, to where she is today: finding joy in the simple things in life, embracing recreational psychedelics, and continuously working on herself while understanding that psychedelic experiences are not the be-all, end-all medicine, and that taking space to integrate learned lessons is where the true potential lies. She recognizes that many of us set out to heal trauma or work on something specific, but often get caught in a “healing trap,” where a victim energy ends up holding us back – and keeps us coming back. When is the healing done? When do these experiences become a habit or escape? What are we not integrating?
She discusses:
and more!
Serving Canada (for now), Kannawellness.com just launched, and features kanna extract eight times more potent than what is on the market today. If you’re curious, use code PT10 at checkout for 10% off your order!
Modern Psychedelics on Spotify
PT308 – Dr. Ido Cohen, PsyD – Vital Psychedelic Conversations
Ipeccoaching.com: Unpacking the 7 Levels of Energy: A Path to Deeper Self-Awareness
PT271 – Jeremy Narby, Ph.D. – Anthropology, Ayahuasca, and Plant Teachers
After the Ecstasy, the Laundry: How the Heart Grows Wise on the Spiritual Path, by Jack Kornfield
You Were Never Broken, by Jeff Foster
Psychedeliceducationcenter.com
*Amazon links are affiliate links, meaning that Psychedelics Today will receive a percentage of the sale
Doctors across the country are beginning to look beyond their prescription pads to explore new treatments for chronic pain management: psychedelics.
As clinical research mounts, patient stories become more frequent, and a desperate call for new solutions to help people find relief for chronic pain becomes louder, substances like psilocybin and MDMA are entering medical education as promising new treatments.
Healthcare professionals are listening and learning how psychedelics could become part of their practices, offering new hope to patients for whom traditional methods – like opioids and nerve blocks – often fall short.

Recently at the annual PAINWeek conference, more than 1,400 pain management professionals gathered to learn about advances in the field. Psychedelics took center stage: the 2024 event marked the first time psychedelic medicines had a dedicated track on the agenda.
Retired FDNY firefighter Joe McKay and advocate Court Wing shared their experiences with using psychedelics to combat their chronic pain conditions.
Presentations in the psychedelic track were delivered by patients, healthcare professionals, including Dr. Eugene Vortsman, licensed clinical social worker Erica Siegal, and attorney Deborah Linden Saly, who are each engaged in research, advocacy, or clinical practice with substances like psilocybin, MDMA, LSD, and DMT.
A growing body of evidence shows people living with conditions including chronic low back pain, migraine, cluster headaches, fibromyalgia, traumatic brain injuries, and phantom limb pain often find that existing treatments are either ineffective or come with troubling or dangerous side effects.
The presence and fervor around psychedelics at the conference is the latest example of a growing focus by the medical community on psychedelics as a new and promising treatment for a wide range of chronic pain and physical conditions.
The complexity of pain is well-matched by the multiple ways that psychedelic substances impact human physiology and perception. Key pain prevention qualities of psychedelics include their ability to interfere with the ascending cascade of pain signals and their powerful anti-inflammatory effects.
Psychedelics can also create neuroplasticity that improves and alters perceptions of pain and corresponding reflexive responses. Many people also report that psychedelics change how they think about their pain and the deeply personal relationship they have with this unwanted constant companion.
New mechanisms of action for how psychedelics improve pain are continually being discovered and proposed. Broadly, it seems to be a complex confluence of biological, psychological and social factors that are all altered by psychedelics. It is premature to state that there is one key or overarching mechanism at work. The field continues to deepen knowledge about which substances and at what doses, are right for which conditions and individual patients.
Another exciting area of exploration is how psychedelics can be combined with a wide array of adjunctive therapies like neuromodulation, physical therapy, massage, mirror box exercises, posture therapy, and more to enhance the efficacy and enduring effect on chronic pain.
For Wing, the success he initially found in psychedelics came somewhat by serendipity after participating in a landmark John Hopkins psilocybin trial for depression.
“I had been evaluated for musculoskeletal pain and dysfunction that I had acquired through a host of injuries over the years of my performance career, and in fact, had just been in the doctor’s office a few months earlier trying to determine if I had arthritis or something worse,” Wing said. “But right there in the (psilocybin) session room, I started having a neurological revision, with my muscles and nerves in my right inner thigh firing in an effort to recalibrate the sensory and motor inputs and outputs in that part of my kinetic chain.”
Personal stories combined with evidence from clinical studies suggest the positive experiences of people in pain who try psychedelic treatments are not lucky aberrations.
Despite a rise in queries, concerns about discussing illegal substances keeps many in healthcare from speaking to their patients about psychedelics for chronic pain.
“Increasing numbers of patients ask me about the potential health benefits of psychedelic agents, both for my area of particular interest – cluster headache, as well as for other headache conditions and for general mental health,” Dr. Brian E. McGeeney, a neurologist and headache specialist in Boston said.
Attorney Deborah Linden Saly cautions healthcare providers: regardless of how state-level laws may change, psychedelics mostly remain illegal Schedule I substances at the federal level. But, she adds, medical professionals can employ strategies to mitigate liability when their clients ask them about psychedelics.
Broadly, healthcare providers can and should be able to answer questions about known efficacy (as documented in the scientific literature), psychedelic-prescription drug interactions, and be able to point to quality sources of information where the patients can learn more. Healthcare providers should be wary of recommending or encouraging psychedelic use until the legal status of these substances changes, but this does not negate providing clients, especially those who have exhausted all typical treatment methods, with resources and education – and encouraging them to seek more on their own.

In the past two years, many professional medical meetings have included discussion of psychedelics to treat pain. Earlier this year, Dr. Emmanuelle Schindler spoke at the American Headache Society’s (AHS) Annual Scientific Conference about her positive and significant research on psilocybin for cluster headache and migraine.
This fall, AHS will also host a pre-course titled Psychedelics and Headache Advanced Course at their Scottsdale Symposium. Presenters for this course include the founder and executive director of Clusterbusters, Bob Wold; sociologist and author of Psychedelic Outlaws: The Movement Revolutionizing Modern Medicine, Joanna Kempner, PhD; and Dr. Emmanuelle Schindler and other physicians. By the end of 2024, Schindler will have spoken on this topic at 16 medical and research events in the past two years.
The patient advocacy group Clusterbusters recently held its 19th annual U.S. conference, and due to growing interest from healthcare providers, they introduced a Continuing Medical Education (CME) course for the first time. This addition led to a fourfold increase in the number of attending medical professionals, who came to learn from the cluster headache patient community about effective treatments, including the potential use of psychedelics.
“What a privilege it was to get a better understanding of this community and the disease they tragically share. But it’s for that shared agony that they can make their lives better, along with the lives of countless others. Not to mention all the lives they’ve saved. Now they can count my enlightenment among their triumphs,” said Dr. Stephanie Nahas, a Philadelphia-based headache specialist.
One in five Americans currently suffers with chronic pain. Pain management professionals know better than anyone else (except maybe individuals living with poorly treated pain) that the medicines and therapies currently available are insufficient to deal with the epidemic that is growing in our aging society. Psychedelics won’t soon be a first-line pain treatment or an effective solution for all the people living with pain, but patients are increasingly using and reporting remarkable effects with psychedelics. And their physicians have taken notice.
Within the coming years, pain management professionals will likely begin to be able to integrate psychedelic medicines into their clinical practices. The time to educate them is now.

Cluster headaches are considered to be the most severe pain a person can experience. With scarce research and no funding, citizen-led science has taken over, and sufferers may have discovered the answer: psychedelics.
In this episode, Joe interviews Joanna Kempner, Ph.D.: associate professor in the Department of Sociology at Rutgers University and author of the recently released, Psychedelic Outlaws: The Movement Revolutionizing Modern Medicine.
The book profiles the history and groundbreaking work of ClusterBusters, a nonprofit researching and spreading awareness about what someone named Flash discovered decades ago: that for some people, psilocybin and LSD could stop cluster headaches from coming on. Through early internet message board posts and email exchanges between Bob Wold, Rick Doblin, and others, Kempner pieced together their story. And through attending ClusterBusters meetings, she discovered that a lot of the true healing lies in the bonds formed and the hope people find when seeing something new work for a pain for which science has no answer.
She discusses:
and more!
Psychedelic Outlaws: The Movement Revolutionizing Modern Medicine, by Joanna Kempner, PhD
Not Tonight: Migraine and the Politics of Gender and Health, by Johanna Kempner
Nih.gov: Response of cluster headache to psilocybin and LSD
Allianceforheadacheadvocacy.org: Headache on the Hill
PT336 – Sisi Li, Ph.D. – Porta Sophia: Psychedelic Prior Art
ClusterBusters Inc. YouTube: Psychedelic Outlaws Book Club – Week 1
*Amazon links are affiliate links, meaning that Psychedelics Today will receive a percentage of the sale
In an age where technology has made it easier than ever to reach each other, humanity faces a glaring paradox: people are more disconnected than ever before, and the need for togetherness has never been greater.
Disconnection isn’t just a social or personal issue – it’s a driving force behind the multiple, interconnected crises we’re facing today. This “polycrisis” is a term that speaks to a complex web of global challenges like climate change, social inequality, and political instability, which are deeply intertwined with the alienation we feel from each other, our environment, and even ourselves. We find ourselves caught in a vicious cycle that erodes our ability to innovate, collaborate, and maintain the relationships necessary to solve enormous problems.
But there is hope in psychedelics. As powerful tools that can heal fractures, psychedelics can restore our sense of belonging and connection with ourselves, each other, and the planet. By addressing the roots of alienation, psychedelics can offer a solution to not only individual and collective repair, but also a way to tackle the global polycrisis threatening our future.
Around the world, people are feeling a profound sense of disconnection – socially, culturally, environmentally, and from themselves. Over 60% of adults are chronically lonely, and this number continues to rise. Modern alienation has led to widespread isolation, division, and perhaps most disturbingly, a loss in the meaning in life for many people. It isn’t just harmful for individuals; it also fuels the larger polycrisis we face by undermining our ability to collaborate, innovate, and sustain a healthy relationship with our world.
Here are some of the most prevalent forms of modern alienation:
Many people feel increasingly disconnected from the social groups that used to give them a sense of belonging. While social media seems to connect us, it actually deepens these divides, creating echo chambers where different perspectives aren’t usually celebrated. This divide makes it hard – if not impossible – to create the collective will that’s required to solve global problems. The ripple effect of failing to solve one issue, like social isolation, intensifies parallel issues, like political unrest or “othering.”
As the world becomes more globalized, many people feel estranged from their cultural roots, especially if they live in environments where their culture is underrepresented or misunderstood. Losing your cultural identity can cause people to feel confused and like they don’t belong, weakening the social fabric that’s crucial to building cultural identity worth preserving. The erosion of cultural identity doesn’t just impact people, but it weakens our ability to draw on each other’s perspectives, which is crucial to navigate complex global problems.
Urbanization and modern living have distanced us from the natural world, contributing to a growing environmental crisis. Many people feel disconnected from nature, leading to a lack of appreciation for the environment and a sense of being out of place in the world. This is a particularly deadly example of alienation: when people don’t feel connected to the earth, they’re less likely to try to protect it. We’re now caught in a vicious cycle, in which environmental destruction is perpetuating social and economic instability, and obliterating quality of life for many.
On a more intimate level, many people feel disconnected from themselves, and are living lives that don’t align with their values, wants, or actual needs. We can see it all around us, in each other, and ourselves, manifesting as depression, anxiety, and a deep sense of unfulfillment. When we’re disconnected from our inner selves, we’re less likely to engage in our world, weakening our capacity for empathy, creativity, and resiliency in the face of glaring global problems that need solving now.

Psychedelics offer a powerful solution. These compounds have shown remarkable potential in healing the mind and restoring crucial lost connections: socially, culturally, environmentally, and personally. By repairing these connections, we begin to lay the groundwork for solving some of the most destructive problems plaguing our planet today.
Psychedelics can break down the barriers that fragment our communities. In communal settings, such as retreats or group ceremonies, psychedelics foster a sense of unity and shared experience.
In a 2021 Imperial College London study, researchers studied how group psychedelic experiences can create a profound sense of “communitas,” or deep togetherness, among participants. This shared experience transcends usual social structures, leading to lasting improvements in social connectedness and well-being.
Psychedelics can play a major role in mending fractured relationships: in families, between romantic partners, or even between nations. In romantic relationships, MDMA-assisted therapy has been shown to help couples reconnect and deepen their understanding of each other. On a larger scale, psychedelics could be used to overcome entrenched national dogmas, fostering mutual understanding and peace between nations. The historic Soviet-American science conference at Esalen is a prime example, when new age practices led to a vision of peace during the Cold War.
By rebuilding social connections, psychedelics can strengthen the communal ties necessary to address global challenges together.
Culturally, psychedelics are helping people all around the world reconnect with their roots and heritage.
Indigenous communities have used psychedelics like peyote and ayahuasca in ritualistic and medicinal contexts for centuries. And today, they’re being used to help ensure that Native American youth do not lose the connection to their heritage. Peyote remains a central sacrament to the Native American Church, and has been used successfully to reconnect Native Americans to their language through song and chanting (and reliable religious experiences). In addition to reconnecting many Indigenous people with their spirituality, ceremony is reconnecting them with their language, which is really important because it was lost for so many people as a result of colonization.
Reconnecting to your cultural identity doesn’t just help heal personal alienation, but also improves the diversity of perspectives and solutions needed to navigate the complexities of a globalized world facing multiple crises.
Psychedelics can foster a deep reconnection with the natural world. When people adopt a deep love of nature, it is, in theory, possible to solve colossal environmental problems.
Many who take psychedelics outdoors report a heightened awareness of their connection to the earth. It can inspire people to live more sustainably and commit to protecting the planet. By rekindling our connection to nature, psychedelics can help reverse the environmental destruction that fuels global polycrisis, promoting behaviors and policies that prioritize ecological balance, sustainability, and even regeneration.
A famed 2019 study by researchers Sam Gandy, Robin Carhart-Harris and others known as the Nature Relatedness Study. The findings suggest that psychedelic experiences can lead to significant and lasting changes in personality, particularly in terms of increased openness and nature relatedness. These changes may also be linked to shifts in political views, promoting more liberal and pro-environmental attitudes. This underscores the potential of psychedelics not only for individual growth but for broader societal impacts.
A 1966 study, Psychedelic Agents in Creative Problem-Solving, demonstrated how psychedelics helped scientists solve complex problems, leading to significant technological advancements. Imagine the potential if psychedelic-inspired innovation were applied to environmental sustainability or the development of new, greener technologies. By unlocking new ways of thinking, psychedelics can help us develop solutions that address the root causes of environmental crises, rather than just treating the symptoms.
On a personal level, psychedelics offer a powerful tool for self-reconnection, particularly in therapeutic settings. They can help individuals explore their shadow, confront unresolved trauma, and rediscover their true selves. This process of self-discovery and deep healing isn’t just transformative for the person, but has ripple effects that improve our capacity to address global challenges. When we’re more connected to ourselves, we’re more likely to engage meaningfully with the world around us.
Take the opioid crisis, for example. Psychedelics offer a promising alternative or addition to traditional pain management, and may drastically reduce chronic pain without the need for opioids. This could lead to a significant reduction in opioid use and addiction, alleviating the strain on healthcare systems and helping to reinvigorate families and communities.
We see the ripple effect of personal reconnection and doing deep inner work all over the psychedelic field; using the principles of Stan Grof, Carl Jung, and Internal Family Systems to help individuals participate in this adventure of self-discovery.
In fact, we’re offering our Vital students the chance to specialize in Somatics, Jung and Depth Psychology as part of their certification for the upcoming September cohort. We’re the first education program to offer this kind of specialization, which we think will be really crucial to helping people heal themselves and others.
The potential of psychedelics to heal and reconnect us, both personally and collectively, is immense. But we can only do it if we approach these substances with responsibility, respect, and a deep understanding of their power.
Philosopher Buckminster Fuller once said, “You do not belong to you. You belong to the universe.” Our role is to use our experiences to help others, and psychedelics provide us with the tools to do it.
Psychedelics can indeed reconnect us, inspire innovation and creativity, and help us solve complex polycrisis problems we face as a society. But most importantly, psychedelics remind us of our interconnectedness: that we are all part of a larger whole, and that our actions have ripple effects that extend far beyond ourselves.
While the concept is often unfairly reduced to replacing one drug with another, many people struggling with addictions are proving that there’s a positive link between the use of psychedelics and addiction recovery. Can microdosing be a factor?
In this episode, Joe interviews Danielle Nova: founder of Psychedelic Recovery, founding team member of Decriminalize Nature Oakland, and Executive Director of the San Francisco Psychedelic Society.
As a recovering addict, Nova discusses how working with psychedelics helped her find her way to recovery, and how she’s spreading that knowledge to others through her Psychedelic Recovery program, which focuses more on ‘targeted abstinence,’ instead of the total abstinence model of Psychedelics In Recovery (which works alongside AA’s 12-step program). She believes that it’s extremely important to reframe addiction as a life process or temporary state of consciousness (rather than a life sentence you can’t escape), and that beating addiction is not about constantly being afraid of a relapse, but about evolving to a state of empowerment: that you can overcome it, and that actually, a horrific addiction may have saved you and brought you to where you’re supposed to be.
She discusses:
and more!
She has co-created Microdosing Facilitator Training with Adam Bramlage of Flow State Micro: a first-of-its-kind 4-month program teaching clinicians, facilitators, and coaches about microdosing and how to safely guide others through the practice. The next cohort launches in January 2025.
Microdosingfacilitatortraining.com
Nature.com: Low doses of lysergic acid diethylamide (LSD) increase reward-related brain activity
PT303 – Adam Bramlage – Cannabis, Microdosing, and Our Evolutionary Connection to Psychedelics
How Long Does A Microdose Last? by Elena Schmidt
Nih.gov: Valvular Heart Disease with the Use of Fenfluramine-Phentermine
A recent report estimated that four million people in the U.S. started microdosing in the last year, with many microdosing at work to improve their leadership skills. But most people start their practice alone, which leads to the question: How much do preparation and peer support change the microdosing experience?
In this episode of Vital Psychedelic Conversations, David interviews Tiffany Hurd: microdosing coach, speaker, business leadership advisor, and student in our current cohort of Vital.

After 15 years in the corporate healthcare industry and several years on antidepressants, she started microdosing psilocybin and saw an immediate change in her life, tapering off antidepressants within a few months. She realized that she could blend her background in business development and strategy with microdosing, helping companies (and specifically company leadership) become more vulnerable, heart-centered, and innovative. She has found that the changes in people have (not surprisingly) led to improved employee mental health, better team relationships, and more open-mindedness and authenticity, and likely, a large reason for that is not the microdosing itself, but the increased attention to preparation and integration – two huge factors often not discussed with microdosing.
She talks about:
and more!
Microdosing is one of the new specialization tracks featured in our next cohort of Vital, beginning September 16. If you want to know more, send us an email or attend one of the next Vital Q+As!
Microdosing as a Coaching Tool: Navigating the Path to Inner Truth, with Tiffany Hurd (A PT webinar)
Positivepsychology.com: The Philosophy of Ikigai: 3 Examples About Finding Purpose
Psychedelics in palliative care has become an exciting new framework for people looking to ease anxiety and embrace spirituality, but the concept is not as simple as just providing a substance.
In this episode, Joe interviews Livi Joy: Director of Health and Safety, Existential Palliative Ministry Lead Facilitator, and more at Sacred Garden Community (SGC).
As she screens applicants for SGC (and Beckley Retreats), she talks a lot about the process and the safety measures that are absolutely necessary when using psychedelics in palliative care – especially under the framework of the Religious Freedom Restoration Act. Does the patient have at least one strong support person? Do they need to start or increase therapy? Does their home need to be rearranged due to possible fall risks? How will certain medications muffle their experience? Are they truly physically healthy enough to be able to handle a powerful journey? And also, is the sacrament always necessary?
She discusses:
and more!
Psychedelics Weekly – AIMS vs. the DEA: An Update on the Fight to Reschedule Psilocybin
Editor’s Note: To date, no empirical studies have concluded that psychedelics cure long COVID. Though case study research in this area is ongoing, this article represents one person’s experience and should not be taken as medical advice. For a more comprehensive understanding of this topic, we encourage you to listen to the full episode of our May 31, 2024 podcast, which includes a broader conversation with experts in the field.
Driven by a deep need for relief and guided by curiosity, in 2022 I turned to psychedelics in my battle against long COVID. What started as a mission to manage post-viral symptoms transformed into a meaningful exploration of psychedelic healing, culminating in unexpected relief, and a shift in my life path. This is my story of navigating the challenges of long COVID, the healthcare system, and my own journey to recovery through the use of psychedelic medicines.
While I might not be the typical image of a person experimenting with psychedelics, my situation led me there. A married 40-something suburban mother of two, working in academia and technology, I was an unlikely candidate for a psychedelic journey. Yet, desperation and long COVID pushed me in this direction.
The fear of stigma and the potential impact on my professional reputation initially made me hesitant to share my experience with substances that remain illegal. However, meeting Court Wing, a passionate advocate for the potential of psychedelics in treating chronic pain and long COVID, changed my perspective. I met Court at a Plant Parenthood integration circle for parents using plant medicines. In that session, I discussed my initial experiences with plant medicines, unaware that this would lead to my story being featured in a medical journal, and even mentioned in TIME magazine.

In early 2022, my life seemed on track. I had a great job at a Canadian university, a bustling family life, and I had just started a Ph.D. My husband, Neil, supported my career ambitions as a full-time caregiver to our children. The U.S.-Canada border reopening in early 2022 prompted me to take the kids to visit family in Connecticut.
We were fully vaccinated and took precautions to keep from contracting the virus. But the Omicron variant was still circulating, and at some point before leaving for our trip, we were exposed and became ill.
The journey back to Canada, coupled with an extended isolation and constant scrutiny from health authorities, left me exhausted, stressed, and at a low point in my mental health.
Severe COVID-19 patients often arrive at the hospital already in respiratory crises. I never needed oxygen, but COVID-19 devastated my body and brain in many ways, initially unbeknownst to me. The aftermath was debilitating: I couldn’t think or regulate my emotions, suffered from severe fatigue, confusion, headaches, and a deepening depression. The healthcare system offered little support, with constant changes in my primary care situation and delayed access to a long COVID clinic.
Determined to recover, I initially pushed myself too hard, only to relapse and sink deeper into despair. I then shifted to prioritizing self-care, including meditative walks in the forest, which helped mildly with depression and brain fog but hit a plateau in cognitive recovery.
After a few months, I was finally able to get a referral, and was accepted into the local hospital’s long COVID rehab clinic. I was so relieved that I would finally get proper care. Then the other shoe dropped – ‘getting in’ only meant that I was now on the waitlist. The estimated wait was a staggering seven months.
From then on, I entered reluctantly into a new phase of acceptance. I made self-care my only priority.
Despite the lack of health care, I took my care and rehabilitation into my own hands. I joined long COVID online communities and read the recent research.
My research on emerging treatments led me to anecdotes of psychedelics aiding COVID-related olfactory loss and brain fog. The growing evidence of psychedelics treating depression, anxiety, addictions, and trauma piqued my interest further. Though no clinical trials were testing psychedelics for long COVID, the safety and efficacy in related conditions motivated me to experiment on myself.
My journey led me to a friend and trained guide, Kate, who understood my symptoms due to her own severe traumatic brain injury. Kate guided me through a psilocybin and MDMA-assisted ceremony that became a transformational experience, comparable to the births of my children in its impact. Almost overnight, my anxiety and depression vanished and my cognitive clarity returned. My headaches eased dramatically. The veil of the long COVID fog was gone.
I cautiously eased back into life. I experienced no crashes in the week following the ceremony, and continually increased my exercise until I reached my pre-COVID workout routine. The day I reached my usual 40 laps in the pool, I knew in my heart that I was truly on the path to recovery. Within weeks of this journey, I initiated a progressive return to work.
Over time, I began to see sharing my story as a responsibility to those suffering from long COVID and other conditions that could benefit from psychedelic medicines. My experience has profoundly changed my personal and professional direction, and I am now pursuing studies in Psychedelics and Consciousness at the University of Ottawa.
My greatest hope is that I can contribute in some small way to the launch of clinical trials for the use of MDMA and psilocybin for the treatment of long COVID. My story is mine alone, but hopefully it will serve to inspire others.
In this episode, special guest host Court Wing interviews Monica Verduzco-Gutierrez, MD: professor and chair of rehabilitation medicine at UT Health San Antonio; Joel Castellanos, MD: co-founder and associate medical director of the Center for Psychedelic Research at UC San Diego; and MaryAnn Welke Lesage: a long COVID survivor who reports experiencing drastic improvement in symptoms after MDMA and psilocybin therapy.
As the world slowly recovers from COVID, many people are seeing continued or new symptoms, and while much is still not understood, these symptoms are being categorized as long COVID: essentially a persistent viral inflammation causing brain fog, headaches, depression, and other hard-to-diagnose symptoms. With estimations of as many as 18% of people in the U.S. experiencing this at one point and 6.8% currently dealing with it, could psychedelics – which can decrease inflammation and reset neural networks – help alleviate these symptoms?
They discuss:
and more!
For more info, read Lesage’s article, “How Psychedelics Became Key to My Long COVID Recovery,” as well as the official paper: “Long-COVID symptoms improved after MDMA and psilocybin therapy: A case report.”
Long-COVID symptoms improved after MDMA and psilocybin therapy: A case report
Time.com: The Latest Promising Long COVID Treatment? Psychedelic Drugs
BMJ Journals: Chronic pain and psychedelics: a review and proposed mechanism of action
Uthscsa.edu: Long COVID: A syndrome wrapped in a riddle inside an enigma
Uthscsa.edu: Dr. Monica Verduzco-Gutierrez discusses long-COVID disability before House subcommittee
Psychologytoday.com: Is Serotonin a Cause of Long COVID Brain Fog?
Psychedelics and pregnancy is a highly controversial and often unspoken topic. But beyond the stigma, what does the research, law and culture say about mothers-to-be consuming psychedelics?
As she had done many times before, Leticia Pizano sat in ceremony with her medicine sisters waiting to feel the effects of the four grams of magic mushrooms that she had ingested. An experienced journeyer, Pizano found it strange that 45 minutes later she began vomiting, an effect she was unaccustomed to so early in the trip.
“The medicine just showed me that I needed to get that out of my body because I was with baby,” she told Psychedelics Today.

Still, the mushrooms took effect and led her on a trip she described as beautiful and empowering. The experience enabled her to form a deeper bond with her unborn child. “There’s just a different connection with her; almost non-human,” Pizano says of her daughter, six months old and the youngest of her twelve children at the time of this writing. After her daughter’s birth, Pizano brought her “medicine baby” to every plant medicine ceremony she attended.
For Pizano, participation in community-based ceremony was a motivating factor for her use of psychedelics, and her use during pregnancy was consistent with cultural norms — she is a member of the Sac and Fox and Kickapoo Tribal Nations, where partaking in ceremonies that include plant medicine sacraments occurs all through a person’s life. For most non-Indigenous people, such participation would be unusual and likely stigmatized, perhaps viewed as dangerous or irresponsible.
Yet, as psychedelics enter a more mainstream era, non-Indigenous birthing parents are relying on them as tools for wellness and even lifesaving measures to address treatment-resistant depression, anxiety, PTSD and addiction. Our current paradigms for substance use during pregnancy do not look at psychedelics with a thoughtful, critical lens. A new approach may be required to accommodate the myriad ways our culture has shifted towards turning to psychedelics over conventional treatments and medications for well-being.

Just as with other psychotropics like antidepressants or anti-anxiety medications, birthing parents and their healthcare providers need to evaluate existing information on psychedelics and pregnancy to make informed decisions about whether to continue using them during pregnancy. But seeking information on the web yields few results. And what little information does exist on the topic is often confusing, incomplete and misleadingly shaped by the War on Drugs. One study on pregnancy and LSD – the study most commonly cited online in reference to psychedelics and pregnancy – was published in 1970.
The American College of Obstetricians and Gynecologists offers a blanket statement recommending the cessation of all marijuana use. Other psychedelics are similarly classified into a category of “substances that are commonly misused or abused,” a classification that bears the markings of bias and misinformation. According to the Global Drug Survey, we know that many psychedelic users ingest these substances in a safe, prepared and informed way, and according to longtime drug researcher David Nutt’s book, Drugs Without the Hot Air, psychedelics like mushrooms and LSD are not inherently addictive.
The March of Dimes, a research and advocacy group for mothers and babies, offers an unsourced page last edited in 2016 on their website that reads: “Street drugs are bad for you, and they’re bad for your baby.” The psychedelics included in this category are “ecstasy” and “other club drugs.” This broad categorization fails to account for the therapeutic applications of psychedelics. It also excludes critical factors like set, setting and dosage, all of which make a significant difference in a psychedelic user’s experience.
Mother to Baby provides more nuanced and specific information on psychedelics, but offer inconsistent guidance on the site. One article advises “Other street drugs, like cocaine, heroin, LSD, MDMA (ecstasy or Molly), and methamphetamine, also are harmful during pregnancy.” While the site’s Fact Sheets for both LSD and MDMA state that it is unknown whether the substances cause pregnancy-related problems.
These blanket prohibitions are largely based on the absence of—rather than the presence of—information about how a substance will impact a growing fetus. The medical research canon contains very little information about the effects of these substances during pregnancy, and substantial obstacles exist for this research to take place at all.
Due to ethical and safety concerns, “The research we do have on pregnancy in general—let alone pregnancy with psychedelics or plant medicine—is minimal because we don’t do research in pregnancy for the most part,” says Jessilyn Dolan, a registered nurse, herbalist, hemp farmer and former member of the Board of Directors for the American Cannabis Nurse Association.
Aside from ethical considerations, says Dolan, another challenge is measuring the long-term health impacts to the child of just one substance due to the enormity of confounding factors. For example, is a person who consumes cannabis edibles during pregnancy also consuming caffeine, alcohol, or prescription medication? How might these substances along with the birthing parent’s diet and lifestyle impact the long term health outcomes for the child? And how might the child’s environment, including exposure to toxins, food insecurity, poverty or traumatic life events, play a role in their health as well?
“When we look at pregnancy, breastfeeding and chest feeding and then doing longitudinal studies around kids, we have so many factors working against us to make that research really legitimized and standardized,” says Dolan.
Of the existing research on this topic, most is either outdated or based on small sample sizes. As legal restrictions on these substances shift, this may change. But information about the safety of ingesting substances during pregnancy is still scant, inconclusive and conflicting.
A study from 1968 on nine children exposed to LSD-25 in utero found elevated levels of chromosomal damage compared to a control group. However, none of these babies exhibited any birth defects. This study, with its very small sample size, has never been replicated. It also did not look at long-term outcomes for these children, rendering the results limited in value.
Similarly, an often cited and widely circulated study from 1994 compared 24 newborns exposed to cannabis to 20 who were not; results at 30 days showed that the cannabis-exposed babies actually scored higher on measures of alertness, were less irritable and had better reflexes. But this study, again with a small sample size and never replicated, did not take into consideration the many confounding factors that could have contributed to the results. For example, the study took place in Jamaica where cannabis use during pregnancy is a common practice and is not stigmatized. In addition, the heavier cannabis-using birthing parents were also more educated, more financially stable and had fewer other children to care for, all of which could have impacted outcomes for their babies.
More broadly, research on prenatal drug exposure is often mired in biases. In his book Drug Use for Grownups, Dr. Carl Hart details several problems associated with brain imaging research on people exposed prenatally to drugs. It is easier to get findings published, he says, when they are consistent with the widespread notion that drug use is bad for the developing fetus. In addition, Hart writes the findings are almost never replicated and researchers often ignore their own data in order to draw conclusions that reflect their own biases.
Still, experts in the field like Amanda Feilding, executive director of the Beckley Foundation, a UK-based NGO that funds psychedelic research and supports policy change, remain hopeful about the prospect for more research on the topic
“Scientific exploration could be carried out using animal models, or using naturalistic surveys to get answers from people who are already using or have already used psychedelics during their pregnancy,” Feilding says.

Weighing risks of physical harm to the fetus against physical or mental health outcomes for the birthing parent is one framework for decision-making of this kind. But these calculations are not the only ones a birthing parent will have to assess. Most people who have experienced pregnancy will be familiar with an increase in monitoring by friends, family and even strangers who may feel entitled to comment on body changes, touch the pregnant person’s body without permission, or offer unsolicited advice or opinions on what the pregnant person ingests. Using psychedelics openly may create social stigma and isolation; the anxiety and stress that those conditions create may pose an additional risk for pregnant people.
Pregnant people are also monitored more closely by state and healthcare agencies. The American Academy of Pediatrics and American College of Obstetricians and Gynecologists recommends screening a pregnant person for drugs when they enter prenatal care. Twenty-five states and the District of Columbia require healthcare professionals to report even suspected drug use, and eight states require them to test for prenatal drug exposure if they suspect drug use. In 2014, Tennessee became the first state to pass a “fetal assault” law specifically allowing prosecution of pregnant women who use drugs, imposing penalties of up to 15 years in prison. The legislation was so controversial it was discontinued in 2016, but has been introduced several times since.
Monitoring for drug use, however, happens disproportionately along racial lines. While white and Black birthing parents have similar rates of any drug use during the prenatal period (though the substances used and patterns of use may differ slightly), an often-cited study from 1990 found that Black birthing parents were 10 times more likely than their white counterparts to be reported to health authorities for their drug use.
Some states are actively working to correct these disparities, with mixed results. A 2015 study of California hospitals that adopted a protocol to monitor all birthing parents for prenatal substance use found that it did not impact child protective services reporting disparities.
New York has taken a different approach. In a testimony to the New York City Council from 2020, David Hansell, Commissioner of the New York City Administration for Children’s Services, stated that the agency had actively discouraged health professionals from making reports to them about a child or parent who tests positive for a substance if there is no negative impact on their well-being and instead make a referral to a service agency. While this could theoretically help level out racial differences, the question remains whether the service agencies would be equipped and trained to adequately address the physical and mental health and other needs of a birthing parent using substances.
Vermont has also taken steps to eliminate the reporting requirement for healthcare practitioners treating birthing parents using substances. If a birthing parent tests positive only for marijuana, they are exempt from hospitals’ and healthcare professionals’ reporting requirements to the Department of Children and Families (although if the marijuana use is thought to endanger a child, it must be reported). The marijuana-only exemption in Vermont is informed by the lack of sufficient evidence suggesting that marijuana use during pregnancy is harmful. But similarly, there is a lack of sufficient evidence demonstrating that other psychedelics are harmful.
For birthing parents who do test positive for substances, their risk of losing custody is also informed by structural racism within the child welfare system. According to Dr. Kelly Sykes, a psychedelic integration therapist and child forensic psychologist, disparities exist between legal systems that govern custody and child protection systems. Allegations of abuse, neglect and drug abuse requiring court intervention exist in both systems. However, only parents within the child protection system—which disproportionately impacts poor single parents of color—can have their parental rights terminated and be permanently banned from having contact with their child. Further, all aspects of their parental judgement are subject to scrutiny; they may be randomly tested for substances, regardless of whether substance abuse was a part of their child protection case.

In this landscape of inconclusive, biased, and misleading information, how can birthing parents make informed decisions on this topic? And without information from peer-reviewed, evidence based research, what might drive someone to elect to use psychedelics all the same during their pregnancy?
For some birthing parents, the mental health benefits outweigh the potential risks.
“Psychedelics can reduce anxiety and depression, and can help people cope with dramatic changes in their lives,” said Feilding. “For those reasons, it’s certainly possible that psychedelics could be beneficial for expectant mothers struggling with prenatal depression or anxiety.”
Dolan, who has worked with pregnant people using cannabis to address treatment-resistant hyperemesis, a condition in pregnancy that creates severe and persistent nausea, frames the issue similarly. If anxiety and stress impede on the connection between parent and baby, research shows that “the relationship and connection is just as, if not more important than the little bit of pharmaceutical that’s going to pass through your breastmilk or pass through in utero to the child,” she says.
Being in a safe, supportive community to help weigh those decisions and process experiences in a nonjudgmental way can be very helpful. For someone like Pizano, this community is built into her everyday life. She grew up attending peyote ceremonies for occasions like baby namings, funerals or healing, and the wisdom she relies on comes from a long lineage of oral tradition, passed down by elders.
For those without such a cultural container, more options are emerging for pregnant people in need of support. A recent Psychedelics Today webinar explored the subject of psychedelics and parenthood with Dr. Glauber Loures de Assis, Associate Director of Chacruna Latinoamérica in Brazil. Groups like Plant Parenthood (which this writer founded) and Moms on Mushrooms also bring together parents to speak about topics that are so stigmatized, they’re rarely spoken about with others.
“Obviously safety is still a primary concern when it comes to kids and psychedelics, let alone issues like pregnancy,” says Andrew Rose, who co-facilitates Plant Parenthood. “But the riskiest thing is not talking about it at all. You can’t have good healthy community education without open, non-judgmental communication.”
Without a clear path for more research on the horizon, and with a landscape of confusing information to draw from, birthing parents will likely struggle to find simple answers. Individuals will still need to factor in their own level of vulnerability, which varies greatly based on race and other socioeconomic and cultural factors. Perhaps the answers we seek do not exist within a search engine, but in a patchwork of wisdom from Western medical research, ancestral knowledge and most importantly, our own inner healing intelligence.
Much like the psychedelic experience itself, the idea of ‘spaceholding’ or ‘holding space’ can strike some as a nebulous concept.
The term is largely synonymous with psychedelic facilitation or ceremony leading. When executed poorly, or not considered at all, the consequences can be severe for the recipient.

When the psychedelic kicks in – whether it be psilocybin, ayahuasca, or 5-MeO-DMT – the individual may arrive at a fork in the road where the ego is invited to dissolve. How they navigate this juncture is key to the quality of the experience and managing their passage towards bliss is one of the key areas where a space holder can earn their salt.
With a safe container created for exploration and tools at hand, including mantras, breathing techniques, and attentive coaching, the journeyer is empowered to surrender gracefully through the depths of consciousness (and, possibly, dimensions). In that moment of ego death – should it occur during the trip – the body can experience long overdue relief from near perpetual fight or flight through a state of rest and digestion which promotes healing.
But in a chaotic setting, left unaided without guidance, travelers may find themselves engulfed in waves of fear and discomfort, veering into distress and confusion and finding elusive the state of simply being, without worries.

The best space holders are beacons of guidance and support in the ethereal, mind-manifesting kaleidoscopic landscapes of a psychedelic journey. Their influence can determine the trip’s trajectory, and the best space holders remain discrete until they are called upon, possessing an intuitive sense of when greater direct presence is necessary.
In the uncharted territory of the psychedelic ’20s, as every man and his dog decides to serve toad venom and ayahuasca, the psychedelic community is increasingly emphasizing the need for well-trained facilitators. Initiatives and training programs like Navigating Psychedelics: For Clinicians and Wellness Practitioners aim to help equip those holding space with the skills to compassionately and adeptly facilitate psychedelic experiences for individuals and groups.
“Psychedelic therapy can bring about intense psychological, emotional, and physical experiences,” writes Michelle Anne Hobart, a spiritual emergence coach. It is thus crucial for space holders to be well-versed in trauma-informed practices to mitigate any issues that may arise, remaining calm, supportive and empathetic for their clients.
In a sense, the phrase ‘space holder’ is metaphoric and refers to the creation of an internal sanctuary for the journeyer, through the adept management of their immediate external reality. Common pitfalls of flawed space holders can include a propensity for touch that may lead to intrusive physical contact, or encouraging excessively high doses. These missteps can all take the participant deeper into the experience than they are comfortable with, and risk energetic transference between the space holder and the participant.
Space holders must exhibit sensitivity and awareness, not only in setting the space optimally with appropriate music, smells, and vibes, but also in witnessing, guiding, and comforting individuals throughout their journey.
Otherwise, ceremonies intended to bring about transmutation and recalibration can become potentially dangerous and risk re-wounding participants who turned up to heal. “The ones who are in the role of holding vigil must be as attuned as the survivors of trauma and spiritual emergency themselves have had to be,” adds Hobart.

The participant has effectively given the space holder permission to witness them in a highly suggestible, hyperplastic and defenseless state. “You’re really putting yourself in someone else’s hands in a very, very vulnerable way, even if you’re an experienced psychonaut,” says Dr. Ido Cohen, a psychedelic facilitator and the founder of the Integration Circle.
The space holder may wish to remain as invisible as possible until they are called upon. It can be tricky to know when greater presence is required, and when to simply allow the profound journey of self-discovery and transformation to happen.
An often-overlooked element of space holding is the ability to be completely present with a participant in their process without judgment or having a desire to give advice, according to Victoria Wueschner, president of F.I.V.E. (5-MeO-DMT Information & Vital Education). Deep in the throes of a visionary psychedelic journey, emotions and words shared may inadvertently relate to the space holder, but it is imperative they do not take it personally and instead remain in a state of compassionate detachment.
“When facilitators step into the role of being a space holder, they commit to giving their full attention and presence to the participant by actively listening with compassion, free of personal ego or motive,” says Wueschner.
If somebody feels unsafe, rushed, or judged, it is more likely that negative thoughts and unresolved memories can arise in an overwhelming fashion. The space holder ideally lifts the weight from the participant’s shoulders, and when the path is clear, a protective bubble is created to block distractions and allow greater space for them to dive deep into their psyches and transform their inner worlds. The space holder is their unobtrusive cheerleader.
The key principles of the Zendo Project, which provides harm reduction education and psychedelic peer support services, are trusting, letting go, being open, breathing and surrendering. The organization advises space holders to be calm, meditative presences of acceptance, care, and compassion.
“Promote feelings of trust and security,” they say on their website. “Let the person’s unfolding experience be the guide. Don’t try to get ahead of the process. Explore distressing issues as they emerge, but simply being with the person can provide support.”

Another aspect of space holding that can be neglected is the process of screening individuals to ascertain whether a particular psychedelic experience is suited for their needs, and then helping people prepare. If a space holder does not, at a minimum, offer to conduct a call before the journey day and provide some preparation exercises – such as intention-setting, journalling or meditation – then that should ring alarm bells.
Space holding doesn’t end when the effect of the psychedelic wears off. A key component of the healing process is the integration – a period which can consist of check-in calls, talk therapy, and the provision of a personalized schedule of activities such as spending time in nature and avoiding certain foods.
But, ultimately, everything is rooted in a trusting bond between the space holder and the patient or client, says Dr. David Rabin, a psychiatrist and neuroscientist who co-founded Apollo Neuroscience.
“Holding space always begins with a safe setting, rooted in trust, that helps to create the fertile ground for the seed of healing to grow. Without the trust and safety of the therapeutic alliance, the healing process can be completely shut down.”
In this episode, Alexa interviews April Pride: creative entrepreneur, veteran of the cannabis space, and now, founder of SetSet, an educational platform and podcast (picking up where The High Guide left off) for women curious about psychedelics.
With Alexa about to embark on the journey of motherhood, she asks many of the questions parents working with psychedelics have to consider: How do you overcome the stigmas of being a psychedelic parent? How do you talk to your children about drugs? How do you know if a substance is ok to use during pregnancy?
Pride discusses:
and more!
The microdosing movement is flourishing, fueled by global citizen scientists reporting transformative wellness benefits. Yet, the practice is still an experiment. Most people have no idea what a microdosing protocol entails, what the experience feels like, or how long a microdose lasts. They are simply curious to know if low-dose psychedelics could be a game-changer for their mental and physical health.
This article provides a beginner’s guide to microdosing psilocybin and LSD, exploring research, protocols, and effects, and answering the question: How long does a microdose last?
Microdosing is the art of ingesting low, sub-threshold doses of psychedelics, typically LSD or psilocybin, for mental and physical optimization. Most people turn to the practice to paint their lives with broader strokes of creativity and focus. Others seek to soften the grip of depression, alcohol dependence, and chronic pain.
Words like sub-perceptual, sub-sensorium, and sub-hallucinogenic also describe the microdosing experience. At about one-tenth of the recreational psychedelic dose, microdosing does not significantly alter consciousness. Rather, it delivers subtle or unnoticeable effects. Microdosers who do notice changes report feeling more energized, uplifted, focused, and in tune throughout the day. Others note slight perceptual changes, like sensitivity to light.
Mushroom and LSD microdoses usually kick in within a couple of hours of ingestion and linger throughout the day. One tiny dose can produce ‘afterglow’ effects lasting at least 48 hours. A regular microdosing practice, combined with rest periods, can elicit even longer-term benefits lasting weeks, months, or years.
LSD is far more potent than psilocybin mushrooms, so microdosing amounts differ significantly.
However, optimal levels can easily skew lower or higher and change over time. Microdosers experimenting with the proper dosage can learn more from the Microdosing Masterclass hosted by the “Father of microdosing,” Dr. James Fadiman, and Adam Bramlage, Founder/CEO of Flow State Micro.
Microdosing may seem like a brand new phenomenon, but the modern microdosing era began shortly after 1943 when Swiss chemist and Sandoz Laboratories employee Albert Hofmann accidentally discovered LSD’s psychedelic effects.
A few years later, the first human LSD trial defined microdosing and answered the question, how long does a microdose last? Swiss psychiatrist Werner A. Stoll, MD, in collaboration with Hofmann and Sandoz, tested LSD doses ranging from 20 mcg to 130 mcg.
A few LSD trials occurred in the years following, but political and societal pressures curtailed psychedelic research until the next century.
Finally, the 2010s witnessed a microdosing resurgence, largely due to Dr. James Fadiman and renowned mycologist, Paul Stamets. Their efforts, anecdotal reports, and growing media attention fueled a global movement and reignited scientific interest.
Dr. Fadiman’s website, Microdosingpsychedelics.com, quickly became the the first massive citizen scientists’ database, compiling transformational accounts from microdosers worldwide.
In 2019, the Quantified Citizen app engaged more than 12,000 participants in the world’s most extensive mobile microdosing study. The initiative revealed that “adults who microdose psychedelics report health-related motivations and lower levels of anxiety and depression compared to non‑microdosers.”
In April 2021, one of the first randomized, double-blind, placebo-controlled microdosing studies found that LSD could increase overall pain tolerance by 20% at 20 mcg doses. It also showed how long a microdose might last, determining that 20 mcg was equally impactful at 1.5 and 5 hours after dosing. The finding suggests small LSD doses provide lasting pain relief beyond the peak onset.
However, this study did not address mental health outcomes.
Double-blind, placebo-controlled studies confirming that microdosing improves anxiety and depression are scarce. The few that exist suggest benefits might arise from the placebo effect, where the person feels better because they believe they’ve taken something that should help – even if it doesn’t have active pharmaceutical properties.
However, microdosing advocates argue that double-blind studies are inherently flawed, partly because they occur in sterile medical environments that do not accurately reflect the real world. Imperfect clinical data cannot diminish people’s concrete experiences.
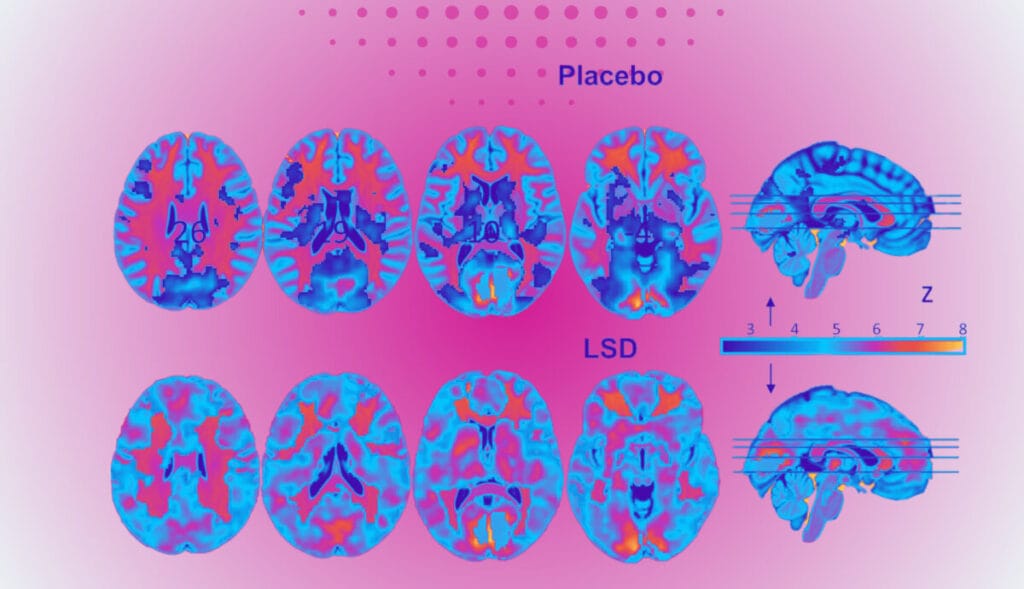
Microdosers report a wide range of experiences based on their psychedelic tolerance, the substance they consume, the dosage, and their unique mental state. Emotional and cognitive shifts typically arise in 60 minutes, with noticeable impacts lasting up to 10 hours. Some people report an afterglow effect up to 48 hours after microdosing.
One pharmacology study found that 20 to 60 mcg of LSD administered intraspinally delivers effects in less than an hour, peaking within the hour and lasting nine to ten hours. However, these results could be skewed because most people do not take LSD intraspinally. Oral and sublingual ingestion are the most common routes.
Fortunately, citizen science reports from sources like Erowid shed more light on the question of how long an LSD microdose lasts.
One Erowid contributor, Tetrisdroid, reported taking approximately 30 mcg of LSD daily for a week for his depression and anxiety.
By the end of the week, Tetrisdroid acknowledged that microdosing LSD might have provided a placebo effect. But either way, he felt better and learned he could go a week without turning to other drugs as a way of self-medicating.
Research suggests psilocybin microdoses should be noticeable within 1.5 hours of ingestion. Studies do not indicate how long the effects persist. However, personal stories reveal a psilocybin microdose can last at least seven hours.
Erowid contributor “Katalyst” experimented with microdosing psilocybin mushrooms for seasonal depression. She started with doses ranging from .2g every four days.
Ultimately, Katalyst decided to continue microdosing on the bi-weekly schedule in future winters.
Clinical data cannot confirm microdosing benefits or their duration. However, participants of a self-blinding microdosing trial indicated that the benefits lasted up to five weeks.
During this timeframe, the microdosers experienced significant improvements in psychological measures such as well-being, mindfulness, life satisfaction, and paranoia compared to baseline. The changes might have occurred due to the placebo effect, but the outcomes were positive nevertheless.
Countless microdosers, including the Silicon Valley elite, have been utilizing intermittent low-dose protocols for years. So, microdosing benefits seem to extend much further than five weeks.

Microdosing protocols are as unique as the people who take them. Frequency and dosages will shift depending on the person and their goals. The only consistent answer to “How often should you microdose?” is not every day.
Daily psychedelic ingestion will cause the body to develop a rapid tolerance. As tolerance rises, microdosers will experience diminishing returns, requiring higher quantities to achieve the same effects.
Most microdosing protocols suggest intermittent consumption throughout the week, along with rest periods, to avoid these issues.
The Fadiman Protocol, or the Beginner’s Protocol, follows a three-day cycle established by Dr. James Fadiman. It distinguishes between microdosing and non-microdosing days so people can take advantage of the two-day afterglow.
The Stamets Protocol, proposed by Paul Stamets, involves more frequent dosing options. These schedules aim to maintain consistent benefits while minimizing tolerance buildup.
The Microdosing Institute protocol suggests microdosing every other day for eight weeks. This method aims to enhance the effectiveness of microdosing for medical or psychological purposes such as depression, social anxiety, ADHD/ADD, migraine, or cluster headaches.
Microdosing offers a nuanced approach to whole-body health through the strategic consumption of low-dose psychedelics. The experience is incredibly mild, allowing people to function like normal. But, the effects are still noticeable, easing anxiety, improving emotional functioning, and minimizing pain for several hours. People who feel called to the practice should continue exploring the research and learning from citizen scientists across the globe.
Learn more about the most microdosing protocols and create your own personalized dosage plan with our Microdosing Masterclass.
In this episode, David interviews Dr. 1Drea Pennington Wasio: integrative physician, psychedelic-assisted therapy facilitator and psilocybin retreat leader, international speaker, podcaster, and author of several books, including Sacred Medicine: Exploring The Psychedelic Hero’s Journey.
She discusses her personal metamorphosis and name change inspired by a powerful ayahuasca experience, and how that moved her into a life more inspired by authenticity and self-love. She gives the details of her retreats, explains her PRISM sessions, and talks in depth about the magic of resiliency: How can we not just return to baseline, but experience post-traumatic growth?
She talks about:
and more!
Her new course on trauma-informed psychedelic therapy begins this month, and her next retreat begins May 10. Head to 1drea.com for details.
“On the fourth cup, I saw these visions and I heard a voice. And you know how it is. Yes, ayahuasca is a hallucinogen, but this voice was so powerful. And it basically was giving me an opportunity to make a shift. And the first time I heard it, I said no. The next night, I was in the same turmoil again, [and] by the time I got to my fourth cup, the voice came back and I said yes. And as soon as I said yes to this horrible question for me, I had to grab my bucket and I started to purge. And with that purge, I could see from me as a baby to that point, it was as if I was purging that timeline. What I realized is who I had become (because I grew up with so much trauma), I felt stuck. I felt like I couldn’t get out of the loop, even with this powerful medicine. And what she gave me was the opportunity to purge that. And by the third time I’m heaving over the bucket, I knew: I’m being reborn.”
“As a physician, I just recognize that without self-love – without true, unconditional self-acceptance, it’s really hard to be healthy.”
“I think everyone could benefit from just imagining: What would life be like if I had more magic, and I wasn’t so blocked and limited by my usual way of being or seeing things?”
“Many of us have wounding based on our family, or attachment wounds, so we need to heal and we need to recover in community. A lot of the people who do find success with 12-steps: they find that we recover together. I think there’s a certain magic that happens. A lot of my colleagues in this space say the group is the medicine. Yes, we take these magical molecules, but the group brings its own sort of medicine.”
Psychedelic Preparation and Integration with Guided Meditations by Dr. DaeEss 1Drea (Special offer)
New course: Trauma-Informed Psychedelic Therapy: Supporting Clients with Preparation and Integration
The Hero with a Thousand Faces, by Joseph Campbell
1drea.com: The Dreamweaver’s Legacy
PT384 – Vital Psychedelic Conversations, featuring: Dr. Dominique Morisano, CPsych & Jessika Lagarde
So, you’ve had a psychedelic experience. And somewhere within the sensory avalanche, the perplexing interior narrative, and avoiding looking at your own face in the bathroom mirror, you (gasp!) may have actually learned something. But what comes next? How can you ensure to take the insights you gathered and apply them to your life? Enter psychedelic integration.
The word ‘integration’ comes from the Latin word ‘integrare,’ which means to make whole or begin again. It also has French roots, from the word ‘intégration,’ which speaks to ‘bringing together parts of a whole.’
While the psychedelic community has yet to uniformly align on a single definition for integration, we can begin to understand it by acknowledging that psychedelics can help disrupt and loosen our rigid personality structures and long-held beliefs. Integration is about finding a middle ground, fixing the tears in our narratives, and becoming whole again.
Sounds simple, right? Simple, yes. Easy, maybe not. Psychedelic integration is both passive and active. It takes time, willingness, and effort to work through and re-live a psychedelic experience within the natural mind. It can involve taking a thorough inventory of the mind, body, and spirit, and challenging oneself to dig deep, get uncomfortable, and sometimes, make big changes.
But don’t panic. Integration is an extremely personal process and doesn’t look the same for everyone. Before getting started, get grounded, give yourself permission to take your time, and treat yourself with love, compassion, and patience.

Someone I used to work with is fond of saying “it doesn’t exist if it isn’t written down.” And while, for our purposes, he uses it in terms of project management, the same is true for psychedelic integration.
As soon as you’ve had a little breathing room from the most intense part of the trip – either before the psychedelic substance has worn off, or a few days after – begin journaling. Writing or recording the parts of the experience that stood out to you is a great place to start while the memory is fresh in your mind.
Whether in a blank notebook, or an intentionally designed psychedelic Integration Workbook, capturing those fleeting thoughts and feelings is often considered a foundational step in psychedelic integration. If a blank page feels a little daunting, check out our comprehensive guide to integrating psychedelic experiences, including meditation prompts, structured journaling exercises, and goal planning.

After a profound psychedelic experience, it’s often helpful to share your story with someone. Whether a therapist experienced in psychedelic integration, a trusted friend, or a member of a psychedelic community, finding a non-judgmental person to hold space for you is important.
The act of verbalizing your experience can help in processing and understanding it on a deeper level. Your experience may have included some anxiety, depression, and discomfort. It’s crucial to find a person who is open-minded (and did we mention, non-judgmental?), allowing you the space to explore your thoughts and feelings without steering them in any particular direction.
If your resources are limited, or there just isn’t anyone in your circle who fits the bill, consider contacting Fireside Project, a free helpline for peer support before, during, and after a psychedelic experience.
“(The volunteers) come to the experiences having had their own experiences, and desiring to hold space for others as they navigate their experiences and navigate their processing afterwards. They’re not doing therapy. They’re not diagnosing. They’re really with the person (the caller, the texter) as somebody who gets it,” Fireside Project founder Hanifa Washington told Psychedelics Today.
Depending on the intensity of your experience and the state of your well-being in the aftermath, finding a trained professional or a doctor may be necessary – especially if you’re in distress.

Psychedelic integration also involves educating yourself about the psychedelic experience. Dive into books, scientific research, and personal accounts that discuss psychedelics and their effects on the mind and body. Understanding the psychological, neurological, and spiritual aspects of psychedelics can provide a richer context to your experience.
To really dig into your integration, consider taking an online course. Navigating Psychedelics: Lessons on Self-Care and Integration was designed so you can learn at your own pace, with lessons on how to get the most out of your experience and integrate psychedelic experiences into your daily life.
These days, there is more psychedelic information available to curious people than ever before. While there can be a lot to wade through, it’s best to find a format that’s easy and compelling to digest. This knowledge can help in recognizing common themes and lessons that emerge in psychedelic experiences. Knowledge is power, and there’s a lot of it out there for you to discover.
Physical health plays a significant role in psychological and spiritual well-being, especially after a psychedelic experience. And if you’ve just had one, your body might have gone through the ringer.
Ensure you’re taking care of your body through proper nutrition, adequate sleep, and regular exercise. Activities you enjoy, like yoga, art, meditation, and nature walks can also be beneficial, helping to ground your experiences in the physical world. Remember, a healthy body is crucial for a healthy mind. Though you may often hear about mental and physical health discussed separately, they are one in the same.

Outside of a therapist or coach, connecting with others who have had similar experiences can be incredibly beneficial for psychedelic integration. Look for community groups, workshops, or online forums where people discuss their psychedelic experiences and integration processes. Sharing with and learning from others can provide different perspectives and insights, and also remind you that you are not alone in this journey.
And even if, for example, you’ve taken psilocybin, don’t discount the experiences of those who have used other substances, from 5-MeO-DMT to ketamine (and all substances in between). While the substances and effects on the body and mind may differ, many of the feelings that can arise and the outcomes can be eerily similar. Finding commonality with many others who use psychedelics for healing and betterment can offer support, understanding, and camaraderie as you navigate your own integration journey.

The morning after my first ayahuasca experience, I woke up to a text from a friend that read:
Try to love the questions themselves as if they were locked rooms or books written in a very foreign language. Don’t search for the answers, which could not be given to you now, because you would not be able to live them. And the point is, to live everything. Live the questions now.
I didn’t fully embrace the sentiment of this quote, originally written by Austrian author Rainer Maria Rilke, until much later. My friend was gently urging me to avoid trying to decode the ayahuasca experience too quickly. I didn’t take this advice, and by the time I landed back in Canada, I decided the medicine was, without question, urging me to live with more gratitude. Maybe so, but maybe that wasn’t quite everything I could have learned, or even the most profound. Because I stopped asking questions, I closed the door to new insights.
“How beautiful that we have this access to deep knowledge of the universe through us, but we have to be quiet. We have to be quiet to hear the whispers of the heart. And when you become quiet, the whispers of the heart become louder and they start filling you in. Then you have to start believing it,” Dr. Michael Sapiro told Psychedelics Today.
Sometimes, psychedelic experiences can be colossal, endless, and enlightening.
And sometimes, they can also be underwhelming, unremarkable, and even boring. Resist the urge to define the ‘why’ too quickly after the substance has worn off. Take a beat, unpack it, and let it marinate in your mind for a bit before concluding its significance – there may be more (or less) there than you think.
Choosing to take psychedelics can be transformative, opening doors to new perspectives and deeper understanding of oneself. But remember, the true journey begins with integration — weaving these profound experiences into the tapestry of your daily life.
While some may choose to take it slow and make the journey completely personal, others might feel inspired to integrate psychedelic work into their professional lives. If that’s you, consider becoming professionally trained before engaging in psychedelic practice with others.
As you navigate this path, cherish the insights, embrace the challenges, and remember that psychedelic integration is meant to be a journey, not a destination.
Eager to learn more? Check out our comprehensive self-paced course, Navigating Psychedelics: Lessons on Self-Care and Integration for your complete guide to understanding and integrating the psychedelic experience.
In this episode, David interviews Saga Briggs: freelance journalist and author of How to Change Your Body: The Science of Interoception and Healing Through Connection to Yourself and Others.
A collection of interviews, peer-reviewed research, and personal story; the book dives deep into the mind-body connection, how to become more embodied, and our need for social connection – which factors into mental and physical health far more than most of us realize. The nod to Michael Pollan’s book is also a challenge: Have we been focusing too much on our minds and now it’s time to pay more attention to our bodies? How much of the benefit of psychedelic experiences is related to truly experiencing our bodies?
She discusses:
and more!
“I think people are familiar with the ways in which different compounds can influence the bodily self, so to speak. And it’s a really interesting idea that that, in and of itself (the modulation of your body or your experience of your body or how the body is represented by the brain): if that maps onto therapeutic outcomes, if that’s part of what’s so beneficial about these compounds – not just changing neural pathways in the brain, but actually giving you a different experience of yourself as an embodied organism in the world – I think this is a really interesting area to look into.”
“The minimal self is kind of just your basic feeling of being in a body, not necessarily tied to your identity. And the narrative self is like the story you tell yourself: who you are when you wake up in the morning, all of your memories, and kind of your life story. And it seems that there’s something going on with psychedelics where the minimal self: its influence sort of traverses over the narrative self, and we get an opportunity to be re-embodied in a way.”
“I don’t see a separation between a place of calmness within my body and the peace of the natural world. It’s the same quality to me. So if I’m standing, looking up at the stars at night in some beautiful remote place, that resonates inside me because it’s the same quality, if that makes sense. I feel it in my body so profoundly because it’s a reminder that my body is part of this greater profound stillness.”
Sagabriggs.journoportfolio.com
The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma, by Bessel Van Der Kok, MD
Multidimensional Assessment of Interoceptive Awareness (MAIA)
Biorxiv.orgThe entropic heart: Tracking the psychedelic state via heart rate dynamics
In this episode, Joe interviews Dr. Peter Grinspoon: primary care physician and cannabis specialist at Massachusetts General Hospital, TedX speaker, certified physician life coach, and author of the new book, Seeing Through the Smoke: A Cannabis Expert Untangles the Truth about Marijuana.
He tells his story of growing up in a house where academics like John Mack and Carl Sagan regularly smoked cannabis, and being inspired by the groundbreaking books of his father, Lester Grinspoon. An outspoken advocate for drug policy reform and embracing different, non-AA paths to recovery, he talks about how he got there: his opiate addiction, fall from medicine, subsequent return, and learning just how deep the stigma against drugs goes, and how much the medical establishment is another arm of the Drug War. Seeing Through the Smoke aims to tell the truth about cannabis, especially on benefits and real and debunked harms. How can we get more physicians and lawmakers on our side if all they know is propaganda?
He discusses:
-The challenge in speaking honestly with physicians about drug use
-Why physicians are in support of researching psychedelics but not cannabis
-Stigmatized language and Drug War vibes in medical software
-The truth about cannabis, schizophrenia, and the risk of drug-induced psychosis
-Portugal and the ‘Rat Park’ model
-The importance of listening to what patients are saying – especially when we don’t have enough good data
and more!
“My dad got John Mack and Carl Sagan together so that Carl can convince John that UFOs aren’t actually real. And apparently, it got very heated, and John Mack yelled at Carl Sagan: ‘You’re being too cartesian!’ So I had a very weird childhood. I mean, all these people were smoking pot frequently in my house when I was growing up, and I grew to associate cannabis with intellectual discussion and very motivated people. I had a very different experience with it than I think it’s fair to say most people did.”
“Back then, the psychiatrists were all completely against psychedelics and people were not at all in favor of medical cannabis. I did my senior presentation as a resident on medical cannabis in the year 2000 (23 years ago), and everybody thought I was so eccentric. And they thought that this was the latest fad, like beta carotene or Omega-3 whatever. And now it’s fun because the same doctors who thought I was eccentric are referring patients to me.”
“94% of Americans support legal access to medical cannabis at this point. …Who’s against medical marijuana? I mean, come on, someone’s dying of cancer; give them some medical marijuana. And again, the AMA still puts it in derogatory quotation marks. So does the American Psychiatric Association. They put ‘medical marijuana’ in these derogatory quotation marks, like, ‘This is just something that only an ignorant patient would believe.’ …I wish they’d just have a little bit more humility and a little bit of interest in rethinking their positions.”
Time.com: Decriminalizing Opioids Will Save Countless Lives
Marihuana Reconsidered, by Lester Grinspoon, M.D.
Psychedelic Drugs Reconsidered, by Lester Grinspoon and James B. Bakalar
Marihuana: The Forbidden Medicine, by Lester Grinspoon, M.D. and James B. Bakalar
In this episode, Joe interviews Dr. Kate Pate: Ph.D. neurophysiologist; Founder and CEO of Coruna Medical; founding board member of the Psychedelic Medicine Association; and Founder of The Way Back, a company that will provide education and coaching services related to military, veteran, and first responder health – often in wilderness settings.
She talks about her introduction to psychedelics through the Heroic Hearts Project, where she later served as an integration coach and director of research, looking at psilocybin for traumatic brain injury symptoms, and how the gut microbiome changes after ingesting ayahuasca. She points out that gut health hasn’t been a focus of research, but it’s now emerging as a key indicator of physical and mental health. So, how do psychedelics, particularly plant-based ones, come into play? Are the long term shifts after an experience related to a change in the bacteria inside of us?
She breaks down what a microbiome is and how it changes based on diet; how inflammation is created and the inflammatory cascade that happens after a head injury; how toxins create a stress response similar to an allergic reaction; the frustrations of vets and the limited resources of the VA; the commonality of substance and alcohol use disorders in people coming home from service; the many nonprofits she’s worked with; and how important it is to increase science funding from the government.
“There’s a very clear shift in the microbiome population in the individuals who consumed ayahuasca, and it seems to be correlated with the improvements seen afterwards. …I do think that, especially with the psychedelics that are ingested and that come from plants, really, there’s a direct impact on the gut, and I think that can be really beneficial. …There’s an experience that lasts a certain period of time, but there are these long-term changes that persist. And what’s mediating that? Is it just the psychological experience, the spiritual experience? Is it physiology? Are we talking about shifts in the gut or other things controlling inflammation? My suspicion is that it’s all of the above, but we can’t negate the physiological component.”
“Gut health and the GI system used to be sort of like this thing that nobody really cared about. It was not the sexy, fun topic. It was sort of an afterthought of like, ‘It digests your food, that’s all it does.’ And now, it’s the star of the show. I mean, there’s so much to understand and learn there that regulates everything about our physical and mental health, that I think it’s really the target of research in the future.”
“If you eat a Western diet and you drink a lot of alcohol, you’re likely going to have the type of bacteria that colonize the gut that thrive in those kind of conditions, which are more pro-inflammatory. So not only can the bacteria themselves signal the immune system directly, but the metabolites that they’re producing can be very inflammatory and toxic. And that can cause leaky gut, it can influence our nervous system, it can influence our immune system. And all of that can affect, ultimately, mental health, because mental health; all these anxiety and depression-like symptoms and disorders are very highly correlated with inflammatory conditions.”
Sciencedirect.com: Psychedelics as potent anti-inflammatory therapeutics
Psychedelicmedicinecoalition.org
Confessions of a Hope Fiend, by Timothy Leary
Here Comes Everybody: The Power of Organizing Without Organizations, by Clay Shirky
Psychedeliceducationcenter.com: Introduction to Psychedelics for Chronic Pain
Do women respond differently to psychedelics than men? And, if so, how are their needs different when approaching these powerful substances?
While crucial research is still limited to help us understand how and why the psychedelic experience might vary vastly among genders, the rise of female-only retreats, clinical settings, and thoughtfully designed psychedelic products and services, are helping provide women safer, more inclusive, and empowering psychedelic experiences.
In an article in MIT Technology Review focusing on women and psychedelics, Juan Pablo Cappello, co-founder and CEO of the ketamine therapy platform Nue Life said, “We started our company knowing that women over 40 are prescribed antidepressants at more than three to four times the rate of men, which has led to one in every five women taking an antidepressant to get through the day.”
Gender differences in the effects of psychedelics remain a topic of mixed evidence, necessitating further investigation. Nevertheless, gender-specific challenges persist. Safety concerns, childcare responsibilities, and the stigma linked to drug use are among women’s hurdles within the psychedelic landscape.
The redesign of healthcare services should prioritize women’s needs. Women frequently experience misdiagnosis and dismissive treatment from healthcare providers, emphasizing the urgency for a more attentive and responsive approach.
One aspect that merits attention is the potential impact of hormonal fluctuations on women’s psychedelic experiences. The menstrual cycle, pregnancy, and menopause can influence the subjective effects and therapeutic outcomes of psychedelics, underscoring the need for tailored research that considers these hormonal factors. Moreover, societal expectations and gender norms place pressure on women, shaping their experiences and interpretations of psychedelic encounters. The struggle to balance femininity, career, and family life can affect a woman’s sense of self and her ability to fully engage in the transformative potential of psychedelics.
With psychedelics being non-specific amplifiers, the external setting, the internal set — the mindset and psychological preparedness of the individual — plays a pivotal role. Women may face self-doubt, fear of losing control, or concern about exposure to vulnerable emotions during psychedelic experiences. Carhart-Harris et al. have emphasized the importance of context, including internal barriers that could potentially hinder the therapeutic benefits of the journey.
Historically, women have been underrepresented in clinical trials across various therapeutic areas, and psychedelics are no exception. For example, the term “inclusion of women” refers to the legal mandate outlined in the National Institutes of Health Revitalization Act of 1993, which requires the involvement of women as subjects in clinical research. This mandate applies to all clinical research funded by NIH unless it is deemed “inappropriate with respect to the health of the subjects,” “inappropriate with respect to the purpose of the research,” or “inappropriate under such other circumstances as the Director of NIH may designate.”
This gender bias limits our understanding of the specific effects, safety profiles, and therapeutic outcomes of psychedelics for women. The limited diversity among research participants has considerable implications for the generalizability and dissemination of treatments. Research suggests that women may exhibit different responses to psychedelics compared to men.
For example, a recent article examined the adverse effects of drugs targeting serotonin GPCRs in the CNS and PNS. These drugs interact with serotonin GPCRs in the brain and various peripheral areas, potentially causing side effects. Estrogen, which is more prevalent in women, influences serotonin synthesis and receptor densities, and drugs targeting serotonin GPCRs disrupt this process. The periodic increase in estrogen levels and the interference with the serotonin system mediated by estrogen could explain why women experience more adverse effects. Women also have lower serotonin concentrations and faster serotonin metabolism than men, which may contribute to the observed differences.
Biological factors, such as hormonal fluctuations, make research on women more complex and, therefore, more expensive. This highlights the necessity of considering gender as a factor in understanding the impact of psychedelics on mental health and well-being. Menstrual cycles, pregnancy, and menopause can influence the subjective effects and therapeutic outcomes of psychedelics. It is also worth consideration that many women experience disruptions in their menstrual cycles. According to the Kaiser Family Foundation in 2022, “most females ages 18-64 (90%) have used contraceptives at some point in their reproductive years, and most have used more than one contraceptive method throughout their lifetime (76%).”
Gender disparity extends beyond research and permeates psychedelic communities, retreat centers, and therapeutic settings. Women may experience subtle or overt forms of discrimination, objectification, or microaggressions, negatively impacting their sense of safety, trust, and overall well-being. Addressing these systemic issues requires a concerted effort to challenge and dismantle patriarchal structures, promote inclusivity, and amplify women’s voices within the psychedelic landscape.
The pharmaceutical industry’s growing interest in psychedelic therapy necessitates a deliberate focus on gender equality and inclusion. As psychedelics become more accepted by the mainstream, it’s essential to ensure that the creation, promotion, and delivery of psychedelic therapies take into account the specific needs of different genders. This entails promoting gender-balanced research teams, conducting gender-sensitive clinical trials, and tailoring interventions to address the diversity of the human species.
While exploring women’s experiences in the psychedelic space, it is also essential to recognize and acknowledge the intersectionality of gender. The experiences of non-binary individuals, as well as those who do not conform to traditional gender norms, deserve attention and inclusion in research and discourse. Non-binary individuals may face unique challenges in navigating psychedelic experiences as they navigate intersecting identities and societal expectations. Let’s foster an inclusive and respectful psychedelic community.
Today, there is limited psychedelic research on factors like drug metabolism, hormonal contraceptives, and womens’ unique physiological traits, hindering the development of tailored psychedelic guidelines and creating unique safety concerns for women who take psychedelics.
Variations in drug metabolism, potential interactions with hormonal contraceptives or reproductive health conditions, and other physiological factors may influence the safety and efficacy of psychedelic experiences for women. Though complex and expensive, funding research focused on women’s bodies and tailoring medicine accordingly will be a game changer.
Certain psychedelics have been associated with increased blood pressure and heart rate, potentially posing distinct implications for women compared to men due to physiological differences. The absence of adequate data raises obstacles in providing accurate information, guidelines, and risk assessments to support women in making informed decisions about psychedelic use.
Studies highlight the relationship between estrogen and serotonin 5-HT2A receptors. Classic psychedelics work by activating serotonin, and research indicates that estrogen enhances receptor density in brain areas governing mood, emotion, cognition, and behavior. This connection may offer insights into gender-based variations in conditions like schizophrenia and depression, more prevalent in women. Additionally, disruptions in estrogen during menopause could affect the 5-HT2A and brain-derived neurotrophic factor (BDNF) signalling pathway, potentially predisposing the brain to depression.
The scarcity of research on women’s experiences using psychedelics to support the process of motherhood and postpartum care poses additional challenges. The limited research perpetuates the perception that psychedelics may pose additional risks to pregnant women or those breastfeeding. Without concrete evidence, caution is often prioritized, leading to a blanket discouragement of psychedelic use during these periods. While caution is essential, the absence of research leaves the potential benefits or risks associated with psychedelic use during pregnancy or breastfeeding unclear, further perpetuating uncertainty and fear.
To address these concerns, there is a need for studies that examine the physiological, psychological, and experiential aspects of psychedelic use in women. Such studies should take into consideration menstrual cycles (including those influenced by birth control), hormonal fluctuations, and reproductive health.

The societal expectations tied to femininity and motherhood can significantly influence women engaging with psychedelics, similar to how men navigate their own situations and societal pressures. These norms shape our human experiences, create additional burdens, and contribute to safety concerns and stigma surrounding psychedelic use. Women may sense societal pressure to conform to traditional gender roles, limiting their willingness to explore psychedelic experiences. Fear of judgment and stigmatization, along with challenges reconciling maternal responsibilities, can constrain their ability to fully embrace the therapeutic potential of psychedelics.
Moreover, internalized notions of femininity can lead to self-doubt, fear of losing control, or concerns about expressing vulnerable emotions during psychedelic experiences. Women may grapple with the balance between societal expectations and personal growth, inhibiting their ability to surrender to the psychedelic experience.
The issue of sexual assault in psychedelic spaces has garnered significant attention in recent years, with instances of misconduct and exploitation reported within the community. Such incidents harm individuals and contribute to the stigmatization and fear surrounding psychedelic compounds. These concerns further emphasize the importance of providing safe and supportive settings, prioritizing consent and boundaries, and promoting gender equality.
While psychedelics hold tremendous therapeutic potential, the occurrence of sexual assault within psychedelic spaces remains a disturbing reality. Addressing conscious consent, creating safe environments, and implementing policies to prevent and respond to assault are crucial steps in fostering a culture of safety and respect.
After movements like #MeToo, female-only spaces have become safe havens for women to explore psychedelic experiences without fearing male dominance and sexual assault. These spaces provide a supportive and empowering environment, allowing women to navigate their journeys free from the constraints of societal expectations and potential gender-based harm. Such spaces recognize the importance of reclaiming agency, voice, and autonomy for women within the psychedelic realm.
Women-only retreats create a unique and transformative space for women to explore their inner worlds, cultivate deep connections with one another, and embark on journeys of self-discovery and healing. Such retreats provide a safe space where participants can fully embrace vulnerability. The absence of men often fosters an environment where women feel more comfortable sharing their deepest fears, hopes, and emotions. This sense of safety encourages authentic exploration and expression during psychedelic experiences, helping women ‘take up space’.
Women-only retreats tend to nurture a profound sense of sisterhood and community. The shared experiences, both during and between psychedelic sessions, can forge lasting bonds and connections. These connections often lead to a deep sense of belonging and support, facilitating sustained relationships beyond the retreat experience.
Women-only retreats also provide participants with the opportunity to explore and reclaim their narratives and identities. Many women join these retreats with experiences of societal and cultural expectations, traumas, and limitations. Psychedelic experiences within this supportive environment can pave the way for self-liberation, empowering women to redefine themselves and their place in the world on their own terms.
Many of these retreats often focus on the exploration and celebration of feminine energy and aspects of the self. This journey can be deeply healing, helping women reestablish a connection with their inner wisdom, intuition, and creativity. Additionally, it can foster a deeper appreciation for the unique strengths and qualities that women bring to the world.
Held frequently in natural settings, many women-only retreats incorporate rituals and ceremonies. Reconnecting with nature and participating in rituals can deepen the psychedelic experience, helping participants feel more in tune with the cycles of life and the natural world. This reconnection can be both spiritually and emotionally enriching, assisting many women in reconnecting with the cycles of their bodies.
In her role as a psychedelic facilitator, Jessika has witnessed women emerging from these retreats with a newfound sense of purpose, self-love, and empowerment. This unique quality of women-only retreats lies in their ability to provide a nurturing and transformative space where women can explore the depths of their psyche, connect profoundly with others, and emerge as stronger, more authentic versions of themselves.
Innovating with women-centered design in mind calls for products and services to be designed for, with, and by women, based on their specific needs. It also requires clearly conveying and enforcing guidelines for respectful communication, boundaries, and consent throughout the process.
The world we live in has been shaped by designers, and it is noteworthy that the creative industry, responsible for much of this design, tends to be male-dominated.
The seatbelt serves as the most cited example of a product designed for men but commonly used by women for safety. Using crash test dummies based on average male sizes and weights has resulted in significant safety disparities for women, making them 73% more likely to be injured in a car accident. Beyond physical safety concerns, women face ongoing challenges related to everyday comfort and practicality. Consider the dilemma faced by pregnant women when deciding whether to position the seatbelt above or below their bellies. Another everyday example is the smartphone, tailored for the average male hand, and transforming into a cumbersome object in the grasp of the average woman.
Taking into account the significant impact of these design hurdles on women’s lives, it warrants a thoughtful approach to designing specifically for women in the context of mind-altering substances. Jemma Campbell, head of U.S. creative of Moving Brands, notes “It is very easy to think that design is aesthetics and aesthetics alone. Design is about much more than aesthetics – it’s about solving real-world problems and improving lives. When done right, it gives brands the ability to build connections with people much like human relationships.”
Focusing solely on aesthetics and neglecting research, strategy, and the overall product experience means you might project your own perspective, adopt codes rooted in learned behaviors and societal norms, and follow cues that may not lead to the best solutions.
“So, when it comes to creating women-only spaces for psychedelic treatment, when patients may feel vulnerable and exposed, we need to fully understand and reflect their unique needs and experiences. And that means women designers must not only be involved – they must be leading the vision,” Campbell says.

Include More Female Designers, Scientists, Researchers, and Engineers
Women buy or influence 85% of all consumer purchases, control 73% of household spending, and make 69% of household health decisions. However, research consistently demonstrates that women are not satisfied with the product and service innovations offered to them. One possible reason: 85% of product designers and engineers are men. In areas like healthcare, where setting and environment are critical, designing with empathy is vital. It’s what makes having diverse design teams so important. Therefore, actively seek the involvement of more female designers, scientists, researchers, and engineers. Diverse teams bring a broader range of perspectives and insights, essential for understanding and meeting the unique needs and preferences of women consumers.
Listen and Learn
Cultivate a culture of inclusivity and diversity within design teams, fostering an environment where women from diverse backgrounds feel comfortable sharing their perspectives and experiences. Actively listen to their feedback, concerns, and ideas, and use this input to drive innovation and product development. Establish a safe and confidential space where women can share without judgment or fear of repercussions. Start small and build it organically.
Increase the representation of women in leadership positions and decision-making roles within design and engineering teams. When women have a seat at the table, they can advocate for designs and innovations that better resonate with female consumers.
User-Centered Design
Prioritize user-centered design principles, ensuring that products and experiences are designed with women in mind. Conduct thorough research to understand their needs, preferences, and pain points, involving women from diverse backgrounds and age groups. The experience doesn’t commence solely upon entering a clinic, retreat space, or product use; it begins with communication. For instance, inviting individuals to observe a retreat to ease them in or incorporating controlled microdosing to facilitate their entry could be part of designing the overall experience.
Collaboration
Collaborate with women’s organizations, advocacy groups, and female-focused communities to gain insights and build strong connections with potential users. These collaborations can lead to valuable co-creation opportunities.
In an ideal healthcare scenario, we envision truly bespoke care tailored to individual needs, irrespective of gender, becoming the norm. While acknowledging the historical challenges and potential future obstacles, we, as professionals, understand the complexities. Yet, as women, we recognize the oversight of subtle but crucial distinctions in female bodies and systems. The lingering patriarchal influence in Western research, product, and system development is a fact. We are now on the journey toward equal opportunities. Undertaking specialized research, embracing user-centered design, and holding space to heal past trauma, we hope to see a more inclusive and supportive psychedelic landscape, where everyone’s distinct needs and perspectives receive the recognition and respect they deserve.
In this episode, Joe interviews Dana Lerman, MD: a decade-long infectious disease consultant who has since been trained in psychedelic-assisted therapy, ecotherapy, and Internal Family Systems, and is the Co-Founder of Skylight Psychedelics, where she prescribes IM ketamine and trains therapists who work with it.
Lerman tells her story: how working with kids with cancer made her want to learn medicine, what it was like working as an infectious disease expert during COVID, and how fascinating it has been to start with modern medicine and then fully embrace the traditional frameworks of ayahuasca ceremonies. She has realized that part of her role is to bring that intention, ceremony, and inner healing intelligence to modern medicine – that that will greatly benefit patients as well as clinicians who naturally want to be healers but are burnt out by the bureaucracy and distractions of the faulty container they find themselves in. Skylight Psychedelics is working on opening a clinical research division, researching psychedelics for Long COVID, and bringing in-person psychedelic peer support services to emergency rooms.
She also discusses intergenerational trauma and how psychedelics have affected her parenting; the impossibility of informed consent in psychedelics and why there should be disclaimers as well as instructions; accessibility, the need for insurance to cover psychedelic-assisted therapy, and why the price of these expensive treatments actually makes sense; why we should be sharing stories of mistakes and things going wrong during ceremonies; and why one of the biggest things we can do to further the cause is to educate our children and parents about psychedelics.
“What’s come to me recently in ayahuasca ceremony is that part of my role in this space is really to bring intention and to bring ceremony and the inner healing intelligence and that concept to the modern medicine space. I mean, there’s so many places for improvement in modern medicine, like even: We have a few minutes for a timeout so you can check to make sure that’s the right patient [and] it’s the right limb you’re going to amputate, but we don’t have a moment to talk about who this person is and the intention of this surgery and what we want for this person. We just have this disconnect, and this disconnect; obviously, it’s not just in medicine. It’s in everywhere. It’s our food. It’s our community. All systems.”
“I have three small children. A lot of why I went to ayahuasca was because I knew [beside wanting] to heal myself of all the stuff that I’ve been carrying around, I wanted to shift my parenting and to be a better parent, and I felt that if I carried my anxiety, my control, all the stuff: It just keeps getting passed down because the kids are just learning from us. But if you can address that, if you can address where does that come from, what is the work that has to be done around it, and do that work, your kids see it. My daughter: When I came home from ayahuasca (she was probably seven); she looked to me and she said, ‘Why didn’t you go there sooner?’”
“Anytime people are using these medicines, I think: There’s a huge disclaimer that should be coming with these medicines, like: ‘Your life will be changed forever. You will never look at anything the same way again, and there’s a possibility that you enter into a space where you are experiencing the vastness of the universe, and that may be very overwhelming for you when the journey is over. You need someone to talk about it with.’ The whole concept of integration is so important.”
Vera.org: John Ehrlichman’s quote about the war on drugs
Uthscsa.edu: Monica Verduzco-Gutierrez, MD
Apollo Neuro: Click here to get $50 off an Apollo wearable!
In this episode, Joe interviews neuroscientist, board-certified psychiatrist, health tech entrepreneur, inventor, and Co-Founder & Chief Medical Officer at Apollo Neuro: Dr. Dave Rabin, MD, Ph.D.
He talks about his path to psychiatry; his realization that trauma and chronic stress were primary themes at the root of most mental illness; and the creation, research and implementation of the Apollo wearable: the first scientifically-validated wearable technology designed to improve energy, focus, and relaxation based on touch therapy. The idea was born from Rabin asking himself: If we’re all starved for touch and constantly feeling unsafe, our bodies prefer a calm, soothed state, and MDMA seems to work by amplifying feelings of safety and essentially telling our brains, “you’re safe enough to heal now,” could a rhythmic vibration programmed to stimulate touch receptors and put our bodies into a meditative state fool our brains into the same perceived feeling of safety – especially if that stimulation is constant? Would our nervous systems be able to tell the difference? So far, the data seems to prove that this technology works.
He discusses what they learned from initial research about how people were using their Apollo wearables; heart rate variability and what changes it; MAPS’ Phase III MDMA-assisted psychotherapy results; the idea of the inner healer; using the Apollo in conjunction with ketamine and other psychedelics to ease pre-experience anxiety; and the concept of MDMA-assisted psychotherapy as reverse trauma, the reality that it could stop epigenetic memory, and the question of whether or not the Apollo can do this on its own.
Apollo Neuro is continuing their research by running 14 different trials right now, and if you ever participated in a MAPS trial, you’re eligible for a free wearable. If you’re just curious about trying the Apollo, you can receive $50 off using this link.
“What we’ve learned through the study of all the work that came before us was that the body actually likes to be in that state. It likes to be in this calm, soothed state, and it’s just overwhelmed and overstimulated a lot of the time and that’s why it’s not in that state. So then the research question was: If we deliver the rhythm that our bodies like to breathe at when they’re at rest (which is like five to seven breaths per minute when we’re normally breathing at 12 to 24 breaths per minute, which is stress breathing), then would the body start to automatically breathe at its ideal rhythm on its own simply by receiving the right rhythm? Is that enough? Like, if you play the right dance beat, will people start dancing on their own or will they just sit in the chair?”
“The word ‘hallucination’ implies that what you’re experiencing is not real, and I hesitate to use that word in the context of psychedelic work because ‘psychedelic’ means to reveal the mind. And so, if we put out the understanding that the revelation of what’s underneath the surface of our consciousness in our minds is not real or hallucinatory, then we might be missing a lot of the meaning of what’s actually underneath the surface.”
“If we are able to show that other safety-based treatments, whether it’s MDMA or traditional ceremonial ayahuasca or other things, or ketamine therapy, or Apollo, or soothing touch: If any of these things are inducing similar changes to cortisol receptors that we saw in that MDMA trial, then we know it’s not the drug that is inducing the healing state. It’s the safety that is amplified by the drug that produces the healing response. And that will be really, really helpful to us as a field to understand what we actually need to heal. I think the theory is [that] we need to feel safe enough to heal. This would actually prove that.”
Apolloneuro.com: studies roundup
The Psychedelic Report: Can MDMA-Assisted Therapy Repair our Epigenetics with Dr. Candace Lewis PhD
Your Brain Explained: Breaking Down Trauma w/ Dr. Gabor Maté & Dr. Rachel Yehuda
In this episode, David interviews Dr. JoQueta Handy, Ph.D., IMD: speaker, author, educator, Natural Integrative Health Practitioner, and CEO and Chief Visionary of Brilliant Learning, Handy Wellness Center, and Brilliant Blends.
She shares childhood memories of growing up on her Grandparents’ farm, where she developed a deep appreciation for nature, staring at the stars, and the beauty in stillness, and how coming back to that stillness has been key in her life and psychedelic journeys. The conversation then shifts to all that she’s learned through her work with children on the autism spectrum: the problems of putting people into boxes; how autism affects everyone; the different ways people learn; the connection between autism and the gut microbiome; and how she has learned more from some of these children than any book could teach her – culminating in a story of discovering that a very challenged child people were ready to give up on could actually read and comprehend everything he was hearing.
She discusses her favorite adaptogens; the art of stacking adaptogens and different modalities; her multi-day coaching sessions; Internal Family Systems; quantum biofeedback; the use of supplements in microdosing; and Brilliant Blends, which sells blends of supplements designed to provide benefits as close to what psilocybin can provide (but legally) – inspired by the unique needs of autistic individuals. PT listeners can receive 10% off all purchases with code: PT10.
“If we look at Western medicine, we are masters at saving lives. We’re not so great at quality of life. And looking more toward Eastern medicine, European medicine: where body, mind and soul [is] more brought into play – healing, working on the mind, the emotional, the mind and the body for a complete healing… So that was really why I chose the path of natural integrative medicine because I did see that everything has a place. Everybody brings a talent to the table. …We, many times, need a village for healing.”
“I’ve had some wonderful mentors along the way, but being on the ground, so to speak – not just in a laboratory, formulating things – being hands-on with those children on a day-to-day basis: that was the greatest teacher of: how is this herb working? How is this adaptogen working? So when I went to formulate Brilliant Blends, I just knew it had to honor them because I was using that knowledge base. I use it on a daily basis with everyone. …Autistic children have taught us what we know from autism, and what we know from autism applies to everyone.”
“That’s the end game. That’s the bottom line in all of this work that we’re doing. That’s where the transformation and freedom is: to realize that this medicine is in all of us. Maybe we’re just using psychedelics to open that door to reveal it and show us the path how to anchor it, but this medicine is in all of us and always was. So if we can use these different pathways, these different approaches to lead us back home, then bravo.”
Mybrilliantblends.com (use code PT10 to receive 10% off all purchases)
Hemplucid.com (use code PSYCHEDELICS10 for 10% off all purchases)
Neurology physician Dr. Burton Tabaac’s interest in psychedelics began almost by accident. He happened upon the topic through a 2019 presentation during his fellowship training at the Johns Hopkins University School of Medicine – and may not have pursued a dedicated interest in the field if he hadn’t attended.
“… In four years of medical school and four years of residency training, psychedelics were not mentioned – not even once as part of a comprehensive allopathic education,” Tabaac told Psychedelics Today.
The Hopkins lecture inspired the physician down a non-typical path for those in his profession: research on the therapeutic potential of psychedelics in treating mental health diseases. Today, he explores psychedelics beyond their traditional association with mental health. Entities inclusive of Parkinson’s disease, dementia, stroke, and traumatic brain injury are of particular intrigue with potential for psychedelics to promote healing, Tabaac shares.
In his recently appointed role for the Mckenna Academy of Natural Philosophy, founded by Dennis McKenna, Dr. Tabaac serves as an advisor for educational pursuits and evidence-based methodology. Through this collaboration, he is dedicated to investigating the possible role of psychedelics beyond their use in the mental health realm, and is passionate about exploring whether these substances could help with functional neurological and neurodegenerative diseases.
“There are specific indications that I feel warrant additional study and funding to assess and discover,” he says. “There has already been a lot of research and literature published dedicated to psychedelics for treating depression, anxiety, addiction and PTSD; I’m very eager to partner in pushing the frontier further to investigate what else psychedelics may have the potential to address.”
In the current landscape of psychedelic research, this alliance highlights the evolving role of physicians stepping beyond traditional methods to investigate alternative solutions. The demand for more research signifies a promising future for psychedelic research, with the potential of extending the possibilities of these substances in treating various conditions.
In the healthcare world, it isn’t uncommon to find that many doctors tend to favor Western medicine while overlooking holistic approaches. Doctors don’t typically embrace integrative routes, because the current medical system is guided primarily by evidence-based research, Tabaac says. Treatments typically require strong evidence of their efficacy before they are widely adopted, which doesn’t bode well for most federally scheduled psychedelics in relative nascent stages of research.
“I also think that having psychedelics as a restricted Schedule I class of drugs prohibits a lot of providers from even being able to offer these therapeutics off-label,” he says. “When you look at where the medical/legal field is heading, there’s a lot of promise with the Phase 3 trial that MAPS has presented demonstrating the potential for MDMA to treat PTSD.”
PTSD patients in the MAPS study received three doses of MDMA, supplemented with psychotherapy. The trial results yielded 50 per cent of participants no longer meeting the criteria for PTSD. One year later, without any additional MDMA doses, the number of patients no longer meeting the criteria increased to 70 per cent, “showing that there is some underlying effect on the brain that is sustainable,” Tabaac said.
The MAPS study highlights the transformative impact that psychedelics – combined with psychotherapy – can have on mental health disorders like PTSD, Tabaac says. As more research emerges, it is expected that the medical community will gradually embrace these alternative treatments and integrate them into mainstream healthcare, ultimately empowering physicians to treat patients with greater efficacy and enriching the field of allopathic medicine.
Back in December 2021, Tabaac stumbled across the Psychedelics Anonymous (PA) platform, a web3 community that shared his enthusiasm for the potential of NFTs to bridge communities of like minded individuals. PA offers a secure environment where members can connect without revealing their identities, utilizing avatars to engage in discussions about psychedelics, and exchange personal or professional experiences.
Membership in Psychedelics Anonymous brought with it additional perks, Tabaac said, offering access to educational opportunities such as a plant medicine course at Cornell and participation in the recent Psychedelic Science 2023 conference in Denver. The project has also established a podcast, The Zero Hour, where Tabaac interviews the top minds in the psychedelic space. The most valuable aspect, Tabaac says, was the connections made with fellow colleagues. He connected with psychiatrists, psychologists, social workers, and researchers who were curious about psychedelic medicine and established this virtual space where they could openly discuss without stigma, judgment, or fear of retribution.
“I attribute a lot of my own development and personal growth and passion for the space to the Psychedelics Anonymous project, because prior to getting involved in that community, there was trepidation over being judged by friends and by society at large, as a lot of the negative press and stigma still remains, dating back to Nixon’s War on Drugs,” he says.
Psychedelics Anonymous also catalyzed Tabaac’s passion in the field to present a TEDx talk discussing Mental Health Meets Psychedelics. In this talk listeners are challenged to question their preconceived notions and judgements as it pertains to the group of restricted therapeutics in the psychedelic class. Tabaac asks if this class of drugs can serve as a paradigm shift in the way mindfulness therapy and mental health is approached.
Dr. Tabaac recognizes the difference between his passion for advancing psychedelic medicine and his commitment to ethics. “I infrequently discuss psychedelics with my patient population, exceptions including clinical trial offerings if inclusion criteria is met. Doctors and health practitioners are constrained by the limits of their medical licensure, and must remain patient until FDA approval is achieved,” Tabaac says. “I think it’s still premature and out of my scope to offer psychedelics to my patients. My mission and my role is better served in pushing clinical research forward, commiting patient enrollment in trials, and inviting speakers who are experts in the psychedelic space to present on my podcast I incorporate teachings on psychedelics to the medical students that rotate with me as it is the only space where they have exposure to learning about these modalities. The enthusiasm and interest among the next generation of physicians is encouraging.”
The demand for alternative mental health solutions continues to increase. Organizations like the Psychedelic Medicine Association, dedicated to providing ketamine treatments and with whom Tabaac is affiliated, are addressing the needs of individuals seeking non-traditional routes. While certain prescriptions may fall beyond the scope of some physicians, adopting a holistic approach becomes crucial. With physicians like Tabaac considering various facets of a person’s well-being, such as sleep, lifestyle, nutrition, social support, mindfulness practices and physical health, individuals can benefit from more comprehensive and personalized mental health care. This avenue goes beyond medications, recognizing the broader needs of patients. It underscores the importance of tending to various dimensions of a person’s life to foster holistic well-being and empowers individuals to explore diverse modalities for emotional harmony. Tabaac emphasizes the moniker of focusing “mental health as part of whole health.”
For physicians like Tabaac, exploring the uncharted waters of psychedelic medicine opens up new possibilities for patient treatment and professional development. It provides access to innovative therapies, nurtures professional growth, and enables them to explore new frontiers beyond the constraints of conventional methods. By breaking stigma, advancing the field, and advocating for holistic modalities, physicians have the opportunity to play a pivotal role in enhancing the field of mental health and allopathy, offering new hope and potential healing pathways to patients. A new era in Western medicine, where evidence-based methodologies, holistic approaches, and comprehensive care intersect, holds the potential for a transformative landscape on the healthcare horizon.
In this episode, Joe interviews one of the world’s leading experts on human performance: New York Times bestselling author and Executive Director of the Flow Research Collective, Steven Kotler.
Kotler’s work explores the neurobiology of peak human performance, flow states, and aging, and the concept of getting our biology to work for us rather than against us in our later years, by using the parts of our brains that expand in our 50s, combined with neuroplasticity, learning by play, and the biggest factor: working toward a very difficult – but not impossible – task. His 30-year exploration of the neurobiology behind people accomplishing ‘impossible’ feats led him to test his theories by teaching himself to park ski at 53 with resounding success, then using his protocol with people up to 70 years old the next season. The story is told in his newest book about challenging tired concepts of aging, Gnar Country.
He discusses the power of flow states and how much flow actually amplifies productivity, motivation, wisdom, empathy, and more; why dynamic motion is a key activity for greater longevity and why skiing and similar action sports are some of the best examples; why dynamic activity in novel environments is even better; why changing one’s mindset may be the biggest factor toward change; why corporations are looking at flow training and where these concepts could go in the future; and of course, how this all relates to psychedelics.
“If you study flow science, it turns out that flow is really great at helping us go from zero up to Superman. It’s also really great at helping us go from seriously subpar, ‘I’m completely broken and sick’ back to normal. And it turns out this combination is phenomenal in the second half of our lives. And flow sits at the heart of peak performance aging.”
“The only way I can go [from] A to B with this is to take everything I know about flow science and peak performance and see if I can use it to accomplish this so-called impossible task. So that’s what the book is. And yes, I was obviously very successful. I went 0 to 60, as I said, in a single season. It was the fastest I’ve ever actually learned anything.”
“The place you’ve got to begin is mindset. The mind-body connection gets tighter and tighter and tighter over time, and it plays a significant role in aging and peak performance aging. Mindset is the greatest example. …A positive mindset towards aging – ‘I am thrilled with the second half of my life; my best days are ahead of me’ – translates to an additional eight years of healthy longevity. It’s wild. …You could be morbidly obese and have a shitty mindset towards aging. Change your mindset, you’ll live longer. Don’t lose weight. Change your mindset. It’s more important. In fact, changing your mindset is more important than quitting smoking for healthy longevity.”
When the Impossible Happens: Adventures in Non-Ordinary Realities, by Stanislav Grof
The Structure of Scientific Revolutions, by Thomas S. Kuhn
In this episode, Joe interviews Oliver Carlin, Founder of Curative Mushrooms, a grow kit solution company designed to produce mushrooms of one’s choosing within 30 days with little effort and no growing experience.
Carlin tells his personal story of 20 years in the Navy to a 7g psilocybin journey and the work of perfecting these grow bags; how a grow bag works; how easy it can be to grow your own mushrooms; the advantages of growing your own mushrooms vs. buying them; the legalities of grow kits and how he has been able to do this; steps growers can take to reduce their legal risks; the variety of people benefitting from mushrooms (especially in the veteran community); and how growing your own mushrooms seems to make the experience more curated and special.
Curative Mushrooms recently hired someone to create new strains for them every month, they do bimonthly live Q&As for people interested in growing, and they ship a bonus mycology book with each kit that shows how to study spores. They offer growing kits for Lion’s Mane, Turkey Tail, and Shiitake mushrooms, but his most popular option is the “All-in-One Happy Mushrooms for Sad People” kit.
“I do believe there’s always going to be a market for growers, because it’s just fun. And you can create your own strains of mushrooms if you really get into it. I mean, you can even name strains after yourself. And plus, isn’t it cool to grow your own, because now you have super fresh mushrooms, you know exactly what it is, how fresh, it’s going to be the most potent because you just grew it, and I’ll be honest, when you grow your own, it feels like the mushrooms were, like, grown specifically for you. I don’t know, there’s something special about them.”
“I didn’t take mushrooms because I was specifically doing it to overcome depression or anything like that. The reason I took mushrooms was: it was like answering questions about the world that I’ve always wanted to know. I’ve always had a problem with everything I’ve been told, and this was my opportunity to finally get some type of an answer for things that I didn’t understand. And that was my reason. And it completely changed my life.”
Curativemushrooms.com (purchase using our affiliate link!)
Curativemushrooms.com: Content Hub
Join us for A Vital Journey: Transpersonal Breathwork Retreat in PA, July 28
In this episode, Alexa interviews Rachel Clark: Education Manager for DanceSafe, a public health nonprofit specializing in serving people who use drugs and their communities.
As we move into the prime festival season, more people are going to be doing drugs, and the importance of harm reduction and drug testing becomes even more central to the experience. She discusses the complications of drug testing and how it’s more of an act of ruling substances out rather than determining purity; the fentanyl problem and its surrounding myths; how to identify and treat an overdose (and what not to do); Philadelphia’s struggles with Xylazine highlighting the problem with regional cross contamination; and DanceSafe’s “We Love Consent” and “Healing is Power” campaigns, which aim to open up the dialogue of true harm reduction and safe spaces outside of the substance alone.
Check out DanceSafe.org for more info, and use this link when you’re ready to make a purchase!
“You’re looking for red flags and not green lights. You’re not looking for confirmation that something is in your substance, you’re looking for a red flag about whether something is obviously or potentially not what you expected.”
“The three major symptoms of opioid overdose are very, very slow, shallow, and or stopped breathing, reduced or absent consciousness, and pinpoint/constricted pupils. And I want everyone to understand that the cause of opioid overdose is when your respiration, your breathing slows to the point that your tissues are not being oxygenated and perfused and your heart stops. That is the sequence. …If people understood that this is about a lack of oxygen because your breathing is too slow, I think that the public understanding of fentanyl overdose and opioid overdose would change a lot, because that, in and of itself, gives you a lot of information when you’re looking at someone and evaluating if an opioid could be involved.”
“Always communicate the limitations of what you know. Assume that you are missing information, because you are. And when you are reporting on something that you witnessed, share only what you saw and what you did, including timelines. This is a major, major note for anybody, especially people who work in EMS, because there have been a lot of very well-intentioned folks who have ended up spreading misinformation like wildfire by saying things as certainties instead of sharing observations.”
Dancesafe.org: We Love Consent
Dancesafe.org: Healing is Power
Energycontrol-international.org
Check out the Lumenate app, and download it through the App store here!
Planning on hitting a festival this summer? You’re not alone. With COVID restrictions and cancellations now a thing of the past, many music lovers are heading back into the wild and hitting summer concerts and festivals all around the world with renewed energy, making up for lost time with their psychedelic communities and their favorite artists.
But with the freedom and joy that comes along with dancing, hugging, and partying with thousands of strangers until the sun comes up, also comes the potential for mishaps, and at worst, serious harm to you and your friends.
Gathered from our team at Psychedelics Today – who have decades of festival experience between them – here are some tips to help you stay safe and get the most out of your party time during this psychedelic summer.
In 2023, there is no excuse for having to resort to taking whatever substances you can get your hands on at a festival. While it’s possible (and likely!) you’ll be offered psychedelics at festivals, never take anything from someone you don’t know. Should you choose to take psychedelics (or any other substances), acquire them ahead of time from sources you trust and test them before consuming any. Groups like DanceSafe, Qtests, Bunk Police, and Test Kit Plus offer a wide variety of regent testing kits to give you a better understanding of what is (and isn’t) in your substances, including fentanyl. And if you’re in Canada, you can send a sample of your substance to getyourdrugstested.com for a free analysis. You can also browse their results catalog to get a sense of what’s going around in your area, and what the lab results reveal. Many festivals partner with harm reduction groups to provide substance testing on-site, so if you can’t test ahead of time, check to see if your festival offers on-site testing – and use it.
Figuring out how you’re getting to – and perhaps, more importantly – from the festival grounds ahead of time is crucial. This may include public transportation, shuttle services, or carpooling, so determine which option suits your needs and budget. Assign a designated driver, don’t get in a vehicle with someone who might be intoxicated, don’t drive if you’ve been consuming, and avoid walking or biking on poorly lit roads or paths. And when in doubt, call your parents – even if you’re 35, chances are they’ll be happy to give you a safe ride home (and they might even make you breakfast).

Upon arriving at the festival, get a map of the grounds and familiarize yourself with its layout. Locate important areas such as the first aid tent, water stations, restrooms, camping area, and stages. Knowing where these facilities are will save you time and effort when you need them most. Pay attention to emergency exit points as well, ensuring you have a plan in case of an emergency.
Preparing a well-thought-out festival survival kit will make your experience much more enjoyable. Some essential items to consider packing include:
Energy bars or nutrient-dense snacks: these will provide quick bursts of energy to keep you going during long sets.
Toiletries: pack travel-sized toiletries to keep your body clean. Wet wipes, hand sanitizer, mouthwash, and tissues are particularly useful in festival environments where you can get real grimy, real fast.
Changes of clothes and socks: staying fresh and dry is crucial in preventing discomfort, blisters, and skin irritation.
SPF protection: apply sunscreen liberally to protect your skin from harmful UV rays.
Pain relievers: bring some over-the-counter pain relievers like Advil or Tylenol in case of headaches or injuries.
Upset stomach relief: bring TUMS or Pepto in case of heartburn or indigestion.
Phone charger or battery pack: keep your phone charged at all times to stay connected with friends and have access to emergency services if needed.
Sunglasses: shield your eyes from the sun and prevent eye strain caused by bright lights or lasers during performances.
Just like you might with a ceremony, or guided psychedelic journey, ask yourself what you’re hoping to achieve before you dose. Is it a greater connection with your friends and community? Is it a deeper exploration of your inner mind and heart? Is it appreciation for the musicians, artists, or to experience the music more intensely? Or is it simply celebration, unwinding, and feeling good? Whatever it is, big or small, it’s ok! Just try to define it, and go into your experience knowing what you hope to achieve. It also helps to tell your friends what your plan is for the evening or weekend (both the substances you plan to consume and your goals). Added transparency can help you with your psychedelic integration, but can also help mitigate any potential harms, if your friends are watching your back and know your consumption plans.
Attending a festival with good friends is not only more fun, but helps keep you safe. Try to make sure you always have a sightline to your friends in the crowd, but develop a plan to find each other in case you get separated (which can happen easily). Pre-designate a central meeting point to wait for your friends if you get separated, just in case there’s no cell service or one of your devices dies. If you’re attending alone, consider joining or creating a meet-up group to connect with other people, so you’ll have at least a few festival friends. Whatever you do, don’t leave the event with strangers – even if they seem nice, or you’re hoping to hook up – you really don’t know who you’re going home with. Grab that number, and hit up the person in a few days instead.

Summer festivals often take place under the scorching sun, and staying hydrated is paramount to keep the good times flowing. Dehydration can occur a lot more easily than you might think, and can lead to fatigue, dizziness, and even heatstroke – a potentially life-threatening condition. Make it a priority to drink plenty of water throughout the day. Carry a refillable water bottle and take advantage of water stations if available at the festival grounds, and consider bringing electrolyte-rich drinks, or drink powders to replenish essential minerals lost through sweat. Pro tip: Bring an extra bottle cap with you. Refillable water stations aren’t always available and venues usually sell water bottles without caps. Being able to seal your water can make all the difference in the world.
When you’re really feeling the vibe, it’s tempting to dance non-stop. However, it’s crucial to give your body regular breaks. Even though you might feel like you have the stamina to go all day or night, dancing for hours on end can exhaust you physically and mentally – and you might not realize it until it’s too late. Take short breaks between sets in shaded areas to rest and recharge. Find a spot where you can sit down and relax while enjoying the music from a distance. Taking regular breaks will pay off – it ensures that you can last throughout the festival without feeling completely drained by the end of the first day.
And speaking of completely wrecking yourself the first day – you don’t want to be that guy. You the one we mean – the guy who’s rolling around naked in the mud a couple of hours after the gates open. Not only is it not a great look, but if you go too hard, too fast, you could spend the rest of the weekend feeling like shit in your tent and miss out on all the great acts you wanted to see. Finally getting to that big event you’ve been waiting for feels incredible, and the urge to go completely off the rails is real (we’ve all been there!) but the best festivals are a marathon – never a sprint.
Amidst all the sets and activities, it can be easy to forget about eating, especially when substances are involved that suppress appetite. And sometimes, eating is inconvenient – vendors might run out of food before the event ends, or pricing for simple snacks or bottled water can cost a lot. However, proper nutrition is essential for maintaining your energy levels. Try to pack a variety of portable snacks like granola bars, nuts, dried fruit, or energy bars. Incorporate water-rich foods into your diet, like watermelon, oranges, or berries to help you stay hydrated while providing essential vitamins and minerals. And if you eat from the food carts, look for options that offer a balance of proteins, carbohydrates, and vegetables to keep your energy levels stable.
Sometimes, the combination of psychedelics and an intense festival environment can be extremely overwhelming. Should you find yourself in an uncomfortable headspace, surround yourself with people you trust, breathe through the emotions, and just remember – it won’t last forever. If a friend is going through a tough time, sit with them, let them know you’re there for them, and remain calm, and hold space. However, there is a difference between a challenging psychedelic experience, and a serious medical issue, so ALWAYS keep a watchful eye out for signs of drug toxicity in yourself and others (nausea, difficulty breathing, chest pain, dizziness, etc.) and seek out medical attention if necessary. When in doubt, a trip to the medical tent is never a bad idea.
Dancing and standing for long periods of time can strain your muscles and lead to discomfort. Take breaks to stretch and release tension. Stretching exercises can improve circulation, prevent muscle cramps, and help you stay flexible. Consider incorporating gentle yoga poses or basic stretching routines into your festival experience to keep you limber and feeling good on the dance floor.
Finding moments of tranquility from all the festival stimuli can be crucial for recharging and regaining focus. Seek out quiet places within the festival grounds:
Chill-out areas: many festivals have designated chill-out zones where you can relax and escape the noise. These areas may feature comfortable seating, hammocks, or shaded spaces. Take advantage of these spaces to unwind, socialize with other festival-goers, or simply enjoy a moment of solitude.
Natural surroundings: if the festival grounds allow, explore nearby natural areas. Find a serene spot under a tree, by a lake, or on a hilltop to enjoy some peace and connect with nature. Nature has a calming effect on the mind and can provide a much-needed break from the intensity of the festival atmosphere.
Silent disco or acoustic sets: some festivals offer silent discos or acoustic sets, where you can enjoy music with headphones or experience stripped-down performances. These intimate settings provide a break from the overwhelming sound levels of main stages while still allowing you to enjoy live music.
Unpopular opinion: acting on the phrase ‘I can sleep when I’m dead’ is, while kind of true, a really great way to ruin your festival experience. Adequate sleep is crucial for recharging your body and mind, so try to establish a sleep routine if you’re on a multi-day trip. Find a quiet and comfortable place to rest, whether it’s in your tent or a designated camping area. Invest in earplugs, an eye mask, some CBD (visit our friends at HempLucid for 10% off all products with code PSYCHEDELICS10) or noise-canceling headphones to create a peaceful sleeping environment, and get some shuteye – even just for a few hours.
What are some of your top tips for staying safe and having a great time at festivals? Join in the conversation on our socials, and tell us how you make the most out of your trips.
In the second episode of our special, two-part series, the Psychedelic Morning Show, Joe Moore and Anne Philippi are live once again bright and early from Psychedelic Science 2023 in Denver. Listen to this podcast as they interview four guests working on the front lines of psychedelic research, law, and the treatment of chronic pain.
Guests for this episode include:
Imperial College London Centre for Psychedelic Research
Clusterbusters
PT404 – Clusterbusters: The Horrors of Cluster Headaches and the Miracle of Psilocybin
Court Wing – Pain and Its Relationship to the Mind
Surprising Results: Psilocybin Trial for Depression Alleviates Chronic Pain, by Court Wing
Psychedelics Today is reporting live this week from the industry event of the year, Psychedelic Science 2023 in Denver. Listen in to this podcast as our co-founder, Joe Moore, and New Health Club founder Anne Philippi hit the conference floor bright and early in the first episode of a special two-part series, the Psychedelic Morning Show.
In this limited series, Joe and Anne chat in real-time with guests working in all corners of the psychedelic ecosystem, from advocacy, law and finance, to research and therapy.
Guests for this episode include:
Working Weekends at a Psych ER – Interview with Julie Holland on NPR
American Psychedelic Practitioners Association
PT249 – Hadas Alterman, Serena Wu, and Adriana Kertzer of Plant Medicine Law Group
Psychedelic Medicine Coalition
PT396 – Moms on Mushrooms: Motherhood and Psychedelics Inside a Broken Culture
In this episode, Joe interviews Priyanka Wali, MD: board-certified practicing physician in Internal Medicine, MAPS-trained psychedelic facilitator, comedian, and co-host (with Sean Hayes of “Will & Grace” fame) of the HypochondriActor podcast, where they discuss interesting medical issues in a funny (and hopefully uplifting) way.
She talks about recognizing and protecting the humanity of healthcare professionals, and how medical school is creating a cycle of hurt people trying to help other hurt people. She believes we need to become more holistic, especially in embracing Indigenous ways of thinking, as their frameworks may be the only way to explain phenomena with which Western science can’t yet come to terms.
They talk a lot about ancient psychedelic use: the use of a soma described in the Rigveda; Egyptian culture and mushrooms observed in statues; Plato; the work of Brian Muraresku and Graham Hancock; and Vedic chants, Kashmiri Bhajans, and how singing (especially in a group) can be especially healing to the nervous system. And as Wali experienced first-hand the Kashmiri Pandit genocide of 1990, she discusses how much colonialism has changed cultures, and how much our cycles of oppression relate to our collective inability to experience pain and fear.
They discuss the psychological impact of living through major catastrophes; the special and hard-to-describe feeling of returning to your home (especially in a world changed by colonization and constant conflict); the sad case of Ignaz Semmelweis and hand washing; ghosts of Japan’s 2011 tsunami, the concept of ‘future primitive,’ and more.
“We’re only thinking about it from a certain perspective. And this is where you think about principles of colonization come in: looking at things only from one perspective. If you start to bring in Indigenous systems [and] Indigenous ways of looking at data, then suddenly, we do actually have ways to account for these other phenomenon that can’t be objectively tabulated.”
“In traditional Kashmiri culture, it was routine to gather together and sing together. We humans: we’re supposed to gather around the fire and dance and chant. There’s actually something very healing for our bodies. And let’s not forget how our nervous systems regulate with each other, so being physically together as a group, as a collective, singing, using our bodies: it’s actually very healing for the nervous system. We need more of that.”
“I think the next shift in consciousness is recognizing that we experience fear as part of the human experience, but we can choose not to give into it. We can be with it, we can allow it to be there, we can even honor it, but we don’t have to act on it. And we can, instead, choose the path of peace or love, or not even choose those paths, but just choose not to do anything with the fear; choose not to oppress someone, judge someone, lash it out, [or] numb it. …Unless we, in the present day, begin to start being with our fear, we will continue to perpetuate these cycles of oppression.”
Apple podcasts: The HypochondriActor podcast
Wikipedia.org: Kashmiri Pandits
Ripleys.com: The Hallucinatory Voices That Saved a Woman’s Life
When the Impossible Happens: Adventures in Non-Ordinary, by Stanislav Grof Ph.D.
Cosmic Trigger I: Final Secret of the Illuminati, by Robert Anton Wilson
Researchgate.net: Evolution of ephedra as the Soma of Rigveda
Tripsavvy.com: Philae Temple Complex, Egypt: The Complete Guide
Sciencedirect.com: The entheomycological origin of Egyptian crowns and the esoteric underpinnings of Egyptian religion (Stephen R. Berlant)
Libcom.org: What is anarcho-syndicalism?
Psychedelics Today: PTSF 35 (with Brian Muraresku)
Netflix.com: Ancient Apocalypse
Psychologytoday.com: Kirtan: The Easy Meditation That Can Improve Your Brain
Paannyaar.com: Kashmiri Bhajans – List Of Most Popular Bhajans In Kashmiri
Psychedelicmedicinecoalition.org
The Structure of Scientific Revolutions, by Thomas S. Kuhn
Npr.org: The Doctor Who Championed Hand-Washing And Briefly Saved Lives
Historicalindia.org: Genocide of Kashmiri Pandits

In this episode, David interviews two of the founding members of Fireside Project: activist, healing justice practitioner, musician, and Chief Ambassador, Hanifa Nayo Washington; and lawyer, aspiring researcher, and Executive Director, Joshua White, Esq.
Fireside Project was created after White volunteered for a help line for years and realized a few things: that follow-up calls made a big difference; that the state of mental health in the U.S. was a disaster (he was talking to some of the same people for years); and that while psychedelics were becoming popular, they would likely only be accessible to the wealthy. Alongside Washington, they realized the most effective thing they could do would be creating a free help line where people could call for peer support during a psychedelic experience, and receive support in integrating that experience afterward. They’ve focused on finding volunteers who may be marginalized or who have been persecuted from the war on drugs, but most importantly, have real experience and true compassion (rather than letters after their name proving their credentials). They are on track to receive 10,000 calls over their first two years.
They discuss Fireside’s Burning Man origin story; the serendipity they’ve seen in the organization’s beginnings and so many calls; where the name came from; how they prepare volunteers; what true equity looks like; and how, while it’s a common challenge for therapists and facilitators to hold back and not try to fix a problem, that may be even more important here.
Fireside Project takes calls every day from 11am – 11pm PST, and while there is an app you can download, they recommend saving their number in your phone for when you need it (62-FIRESIDE). And to destroy the notion of being afraid to ask for help, they encourage everyone to share their stories on social media: the times that you’ve used Fireside Project or the times you had a challenging experience and wish you had known about them. Many newcomers have no idea this support exists, and it could truly be life-changing for them.
“What’s revolutionary about what we’re doing in this idea of democratizing care is that these are volunteers, and they come as peers. They come to the experiences having had their own experiences, and desiring to hold space for others as they navigate their experiences and navigate their processing afterwards. …They’re not doing therapy. They’re not diagnosing. They’re really with the person (the caller, the texter) as somebody who gets it.” -Hanifa
“I think some of the most powerful moments on the line come when we say absolutely nothing at all, when we just allow the silence to become almost palpable, to really feel that ember. I think silence has led to so many of the most beautiful moments that I’ve been lucky enough to see on the line.” -Josh
“By being able to create a safe and non-judgmental space for people by phone, then yes, that absolutely can reduce the risks of their psychedelic experiences. And I think there’s kind of a yin and yang here, which is that when a person is in a space of non-judgment, and when they do feel deeply seen and heard and listened to, then that not only reduces the risks, but it also allows someone to really turn towards their psychedelic experience and to unwrap the gift that’s before them.” -Josh
Year of Yes, by Shonda Rhimes
Good Chemistry: The Science of Connection from Soul to Psychedelics, by Julie Holland (*Josh called it The Chemistry of Connection, but that’s a different book)
In this episode, Joe lets Court Wing take lead in interviewing two of the leaders behind Clusterbusters: Founder and Executive Director, Bob Wold; and President, Eileen Brewer.
A long-time friend of the show, Court Wing has become our resident expert on chronic pain, writing articles about how psilocybin relieved his chronic pain, and hosting Timothy Furnish, MD & Joel Castellanos, MD in their episode about phantom limb pain. Now he speaks with Clusterbusters, a non-profit dedicated to educating people about the horrors of cluster headaches, funding ongoing research into new treatments, and normalizing the miracle that psilocybin has been to so many sufferers in alleviating their headaches.
Wold and Brewer discuss their past struggles (Wold is a cluster sufferer and Brewer has migraine disease) and discovering the amazing intervention of psychedelics; the battles they’ve gone through in spreading this knowledge; how using psychedelics is also helping people work through PTSD; the barriers that legal psilocybin is creating; the concept of schools having a drug education program; the research looking at cluster headaches and other headache diseases; their creation of the Pain And Psychedelics Association, and more. While cluster headache sufferers have a lot to be frustrated about; as psilocybin becomes more mainstream and more and more research is funded, they now have a lot of hope.
“A couple of people started growing their own mushrooms and self-treating themselves just to try it to see if it might actually help, and the results were incredible. It was better than anything that any of them had tried in the past. It wasn’t really an abortive (it wasn’t treating one headache) and it wasn’t really a preventive, where you would take it and you would prevent some of your cluster attacks. It was something that was actually doing both of those things, and people were getting long-lasting results by one or two doses of magic mushrooms.” -Bob
“It makes sense that that would happen within a disease community, it happens outside of disease communities too. Some people just use psychedelics occasionally just to get that perspective back and to work within themselves (and without themselves) to sort it all out, [and] get themselves back together. And I think there’s a real division there between people who do that and people who don’t.” -Eileen
“The two or three years before my first dose of psilocybin, my medical bills were like $20,000 a year trying to treat my clusters. That included hospital stays and specialists and travel. …The first time I grew my own mushrooms, it cost me a hundred dollars to grow a year’s supply and I didn’t have to go to Walgreens to pick up my medicine. So my medical treatment for the following year for my cluster headaches was $100 versus $20,000 and I was able to take as much as I needed when I needed it. And at this point, that’s what most people with headache disorders are doing; they’re growing their own because the system is going to take years and years to be built into something that’s actually accessible to everybody – and affordable.” -Bob
“People are dying while we’re waiting for these policies to happen, and I’m really struggling with the fact that we are setting up more barriers. I know that all the intentions are good, but we are hurting people.” -Eileen
Psychedelics Today: Surprising Results: Psilocybin Trial for Depression Alleviates Chronic Pain
Psychedelics Today: Why Did Psychedelics Relieve My Chronic Pain?
Psychedelics Today: PT306 – Dr. Devon Christie – Vital Psychedelic Conversations
UC San Diego Psychedelics and Health Research Initiative
Newswire.ca: Apex Labs Granted Approval for 294 Patient Take Home Psilocybin Clinical Trial
FDA.gov: Risk Evaluation and Mitigation Strategies | REMS
Yalemedicine.org: Emmanuelle Schindler, MD, Ph.D.
In this episode, David interviews neuroscientist, artist, and educator, Melanie Pincus, Ph.D.; and Ph.D. candidate in Neuroscience, lead or co-author on over a dozen scientific publications, and regular contributor to PT, Manesh Girn.
They tell their stories of how they became interested in neuroscience, and stress the importance of staying radically open-minded (or “epistemically naive”) when it comes to how much we can claim we understand about the brain, the mind-body connection, and consciousness itself – that while fMRI and other advances have brought us a long way, there are still a ton of “unknown unknowns,” especially around creativity, decision making, and imagination. They discuss the misconception that we only use 10% of our brains; comparisons between the brain and the universe; society’s misunderstanding of “happy hormones” (dopamine, serotonin, etc.); how chronic stress takes a toll on all parts of the body; how MDMA works with memory processing; and how stacking modalities with the psychedelic experience (like play or activities focused on emotion regulation) can really help with personal goals and growth.
They have taken their understanding and fascination with neuroscience and applied it to a new course in our Psychedelic Education Center: “Psychedelic Neuroscience Demystified: How Psychedelics Alter Consciousness and Produce Therapeutic Effects“: an 8-week live course with 10 hours of prerecorded material and a built-in community. It was designed with practitioners and clinicians in mind, but with the goal of still being as accessible as possible for anyone who is curious about the neuroscience of psychedelics, and how that knowledge can help with preparation, the journey, integration, and working with a heightened window of neuroplasticity.
Class begins on May 17, and if you sign up before April 12, you can get $100 off!
“There’s so much good science now, and good neuroscience that can inform how people work with their clients in terms of helping them set up for and make sense of their psychedelic experience and ways to optimize the preparation before going into a psychedelic journey, the actual psychedelic journey in terms of thinking about dosing and type of substance to work with, and then also in the integration period, where there’s this heightened window of neuroplasticity and how one could really work with a client to best take advantage of that window of opportunity to lead to lasting change.” -Melanie
“It’s just this blob, this squishy blob of matter. And you think: for that person, their entire life, experiences, memories, [and] hopes were all happening in this little blob that’s in my hand. And just seeing all the layers of blood vessels and how everything’s connected to each other, it’s just fascinating and it’s downright bizarre that somehow, this thing can give rise to experience and consciousness. It’s like, how the hell is that even possible?” -Manesh
“For people who are interested in stacking modalities, there’s other modalities that are really potent at promoting neuroplasticity. So if you want to synergize with the window of plasticity during the integration period, you could for sure partake in regular exercise, because that’s one of the most well-known plasticity promoters.” -Melanie
“How do we respond adaptively to times of change? How do we adjust ourselves? How do we create homeostasis in a changing environment, and how do we adapt to new circumstances? And this is also a whole brain/nervous system/body affair as well, on how to regulate your entire organism to deal with change and to be resilient and to be adaptable. It’s not just in the brain. It’s not just in the brain at all.” -Manesh
Psychedelic Neuroscience Demystified: How Psychedelics Alter Consciousness and Produce Therapeutic Effects (Sign up before April 12 for $100 off)
YouTube: The Psychedelic Scientist
Psychedelics Today: PT258 – Manesh Girn – Psychedelics and the Brain: Neuroplasticity and Creativity
Theguardian.com: Dreamachine, the psychedelic contraption hoping to blow British minds
Huffpost.com: What Exactly Are Sweetbreads, Anyway? A Guide For Anyone Who Doesn’t Already Know
Britannica.com: Do We Really Use Only 10 Percent of Our Brain?
Sciencedaily.com: Massive study reveals few differences between men’s and women’s brains
Healthline.com: How to Hack Your Hormones for a Better Mood
Psychologytoday.com: What Does ‘Allostatic Load’ Mean for Your Health?
Psychedelics Today: PT288 – Annie & Michael Mithoefer – Vital Psychedelic Conversations

In this episode, in celebration of International Women’s Day, Victoria interviews Tracey Tee: co-founder and CEO of Band of Mothers Media, co-producer and co-host of the Band of Mothers podcast, and founder of Moms on Mushrooms, an online educational community for psychedelic-curious moms outside the prying eyes of social media.
With similar histories of womb trauma, self discovery, and body reconnection, Victoria and Tracey discuss the complications of motherhood, substance use and embracing psychedelics in a broken culture, in which engaging with small, approved coping mechanisms is fine – where the “wine mom” archetype and numbing yourself with medications is celebrated, but where we don’t often talk about how challenging motherhood can really be, and the lasting mental, physical, and spiritual impacts of birth, loss, and grief. Tracey’s goal with Moms on Mushrooms is to bring mothers together for personal growth, healing, and most of all, for the safe, supportive container that so many women considering plant medicine need.
She tells her story of creating and performing “The Pump and Dump Show” and the psychedelic journeys that led her to creating M.O.M., and discusses much more: how those large dose journeys reconnected her with her body; how microdosing has helped her feel more vulnerable, honest, and in tune with her daughter; how psychedelics can help parents realize where problematic core beliefs came from; how teaching children the ways of the world forces parents to confront and reaffirm what they truly believe; and the challenges mothers face in even talking about wanting to try psychedelics.
If you’re a mother and this episode resonates with you, check out Tee’s Microdosing 101 (for moms) course or join the Moms on Mushrooms community for $4.44 a month.
“Had I not had this divine intervention, I think I would have been pretty stubborn, which I can tend to be. I would have not wanted to be vulnerable with my daughter because I think I was raised to say that that wasn’t something that is good or that I should show – I’m a parent: ‘My way is the highway.’ Instead, I’m much softer. I ask for forgiveness, I tell her when I screw up, I admit my mistakes, [and] I ask her what she thinks. I always talk about Old Tracey and New Tracey (Old Tracey and ‘Shroom Tracey’): Old Tracey would have never been like that, and I think that’s a real gift, because in asking forgiveness [and] in admitting my mistakes, I’m changing.”
“What is the most upsetting to me is the fear, like this push/pull of hearing either my story or your story or reading How to Change Your Mind or watching a Netflix thing and saying: ‘My soul is telling me this makes sense, my soul is telling me to give this a shot. I might have a way out of this,’ and then my head is like: ‘You cannot do this. You’re a bad person, this is shameful, you might die (which is ridiculous) and at the very least, your children will be taken away from you.’ And that is why I’m talking to you, because that has to stop. It has to stop.”
“I don’t love rehashing the past. I don’t love carrying victimhood, but I am sad for what I lost. And when I work with the medicine (again, intentionally, safely; all the things that we’ve been talking about), I am shown, piece by piece, [that] I’m calling all those parts back. And it’s not easy, but it’s like I’m rebuilding. I’m like a Lego project right now, and I would never be able to do that without the shrooms.”
Psychedelics Today: Reclaiming Ownership of Your Body With Psychedelics, by Jessika Lagarde
Psychedelics Today: PT236 – Drugs: Honesty, Responsibility, and Logic, featuring: Dr. Carl Hart
Psychedelics, once heavily restricted for research, are now being rigorously tested through clinical trials to explore their potential therapeutic benefits. But how are women represented in the search to uncover the efficacy of psychedelic medicines?
While the inclusion of women in psychedelic clinical trials is clearly important – both to understand the effects of these medicines on all genders as well as to develop effective treatments for conditions that primarily affect women – women have historically been underrepresented in clinical trials.
Why has this become the norm? Is it because women aren’t as available as men to participate in studies? Or perhaps women don’t suffer from the illnesses being studied as often as men?
Spoiler: it’s neither.
The clinical trial process is, largely, a series of research studies that evaluate the safety and effectiveness of new drugs, treatments, or medical devices on human subjects. To fit into a pharmaceutical model, a.k.a. develop a drug or treatment protocol that clinicians can prescribe and health insurance will cover, psychedelic medicines must follow the same clinical trial process that all new drugs and treatments undergo.
If it seems like there’s a new clinical trial announced each week – from psilocybin for depression to MDMA for PTSD to LSD for cluster headaches – it’s because these trials are crucial (and non-negotiable) for biotech companies seeking to bring their compounds and modalities to market. These trials aim to prove the effectiveness of a particular compound or method of use, and ultimately secure the holy grail of U.S. Food and Drug Administration (FDA) approval.
Clinical trials are conducted in several phases, each with specific goals:
Phase 1: A small number of healthy volunteers receive the drug or treatment to evaluate its safety and determine the appropriate dosage.
Phase 2: A larger group of volunteers with the condition that the drug or treatment is designed to treat receive the treatment to assess its effectiveness and side effects.
Phase 3: An even larger group of volunteers with the condition receive the treatment in a randomized and controlled study to confirm its effectiveness and monitor side effects.
Phase 4: The drug or treatment is approved and marketed for public use, and ongoing studies continue to monitor its long-term safety and effectiveness.
Throughout the clinical trial process, participants are closely monitored and data is collected to evaluate the drug or treatment’s safety, efficacy, and potential side effects.
As hard as it may be to believe, it wasn’t until 1993 that women and minorities were required to be included in any NIH-funded clinical research. In 1977, the FDA recommended excluding women of childbearing age from Phase 1 and Phase 2 trials, even if they used contraception, were single, or had husbands with vasectomies.
The objective was to avoid unforeseen birth defects in babies born to women in clinical trials. The result, however, is that most currently prescribed medications were approved by the FDA before 1993 – which means they’re prescribed to women and men at the same dose and were unlikely to have adequate representation of women in their clinical trials.
Francesca Minale, President of Vici Health Sciences and an expert at working with the FDA to bring new medications through clinical trials to approval, says the lack of gender differentiation in dosing persists despite known differences in disease states by gender.
“There is a lack of incorporation of gender data and generic specific dosing and administration on FDA-approved prescription labels,” said Minale. “This gender bias in the research needs to be addressed, especially as it is well documented that many diseases, such as mental health or heart disease, are recognized to have gender differences.”
Excluding women from early-stage clinical trials led to a vast shortage of data around how today’s drugs affect women – a knowledge gap that scientists are still trying to fill. Even though the NIH now requires women to be included in all clinical research funded by the government agency, there are still many criteria that make it difficult for women to participate in clinical trials.
The results of clinical trials play a critical role in informing regulatory decisions about whether to approve new medicines for widespread use. However, in the past, clinical trials often failed to accurately reflect the populations they intended to serve – especially women.
This is actually a pretty big problem, because women experience adverse drug reactions nearly twice as often as men. Women consistently manifest elevated blood concentrations and longer elimination times of drugs, unrelated to differences in body weight.
As psychedelic clinical trials seek to determine the safety and efficacy of new psychedelic treatments, it’s imperative we learn from past mistakes. A recent study identified 86 medications approved by the FDA that are more likely to cause complications for women than men.
But yet it’s common practice to prescribe equal doses of medications to men and women – contributing to the overmedication of women and female-biased adverse drug reactions.
In fact, because women were excluded from many pivotal clinical trials, many drugs have been withdrawn from the market or have had their labels changed to include warnings about increased risks for women after they were already approved by the FDA and widely used.
Amy Reichelt, Ph.D., Director of Neuropharmacology at Cybin explained, “In early-stage clinical trials (i.e., Phase 1) where drugs are tested in healthy volunteers, key inclusion/exclusion criteria can bias genders tested.”
Typical protocol wording includes: “Women of childbearing potential (WOCBP) must be non-lactating and have a negative pregnancy test. Females who are not WOCBP must be either surgically sterile or post-menopausal.” Reichelt said. “This immediately excludes a number of women, particularly when age ranges of trials can have cut-offs of 55-60 years.”
Moreover, it is often written into the trial protocol that a woman of childbearing potential must agree to practice an effective means of birth control/contraception during their participation in the clinical trial, and following the trial for several months. This could impact individuals who are trying to start a family for many months, again discouraging women from participating.
Reichelt pointed out, “Later stage trials (i.e., Phase 2b, Phase 3) can be less restrictive as they are testing in patient populations and initial safety tests are fulfilled in the healthy volunteers in early stage trials, but still there are often requirements for contraceptive use that fall upon the women’s responsibility.”
In addition, body weight restrictions may also prevent women from participating if they are below the protocol threshold i.e., less than 60 kg/132 pounds.
The differences between the sexes in circulating levels of sex hormones, such as testosterone and estradiol, can affect pharmacokinetic or pharmacodynamic parameters – which help determine how the drug is absorbed, distributed and metabolized in the body, and how the drug affects the body, Reichelt explained.
Body composition can impact how a drug is processed and eliminated from the body, too. “Women typically have a lower body weight than men, so when the same dose of a drug results in a higher level of drug circulating by body weight. As women generally have a greater body fat content than men, some drugs can be distributed through the body differently,” said Reichelt.
The impact of sex can differ across life stages, too. After menopause, the reduction of estrogen can alter aspects of brain plasticity. Preclinical studies have shown that at the neuronal level, estrogen can increase the density of dendritic spines.
This brain phenomena may subtly affect mood and cognition during a woman’s estrous cycle, and could affect clinical outcomes. More studies are needed to fully understand these impacts, especially when it comes to psychedelic medicines which are closely tied to brain plasticity and dendritic spines.
For Natalie Gukasyan, M.D., Medical Director of Psychedelic and Consciousness Research at Johns Hopkins University School of Medicine, the physiological differences between men and women in the psychedelic experience and outcomes is an area that requires further investigation.
“We don’t yet have a clear understanding of how different biological factors, such as hormonal fluctuations, including menstrual cycle and menopause, may impact the psychedelic experience. However, it does seem that psychedelics may have an impact on menstrual function,” she said.
Gukasyan co-authored a recent study published in the Journal of Psychoactive Drugs on the impact of psychedelics on menstrual function. While the study looked at only three women ranging from 27 to 34 years of age, the results were significant enough to warrant more research.
“Although phenomena related to menstrual and reproductive function have been largely overlooked in the psychedelic literature to date, these effects may have therapeutic utility and warrant further study,” the study concluded.
In the field of psychedelic medicine, where compounds are being extensively studied scientifically for the first time, the underrepresentation of women in clinical trials could have serious consequences for the safety and efficacy of these treatments. Without data on the experiences of women, it is impossible to accurately assess the potential benefits and risks of these new medicines before bringing them to the masses.
By working to increase the representation of women in clinical trials for psychedelics, we can help to ensure that these treatments are developed in a way that is safe, effective, and equitable for all.
Thankfully, many psychedelic clinical trials are moving forward with this ethos. For example, two-thirds of the participants in the MAPS’ Phase 2 and 3 clinical trials of MDMA therapy for the treatment of PTSD were women.
Rick Doblin, the founder of MAPS, said, “When it comes to PTSD, we talk a lot about the veterans, but it’s mostly women who are sexually abused or have childhood traumas that have PTSD. I think that the media attention on veterans sort of distracts people from the understanding that it’s mostly women that we are treating. Two-thirds of the people in the [MAPS] study are women.”
So far, MAPS has administered MDMA to approximately 1,700 human subjects. Their recent Phase 3 clinical trial of MDMA-assisted psychotherapy for PTSD also included an assessment of gender identity beyond the binary male and female gender assigned at birth – an important distinction since transgender and gender diverse (TGD) people experience PTSD at higher rates than the general population.
Other groups conducting clinical trials actively seeking women participants include Psycheceutical Bioscience, which has partnered with clinical research organization (CRO) iNGENū in Australia to conduct its Phase 1 and Phase 2 trials of a topical ketamine cream to treat PTSD.
“iNGENū takes gender balance in clinical trials very seriously and the diversity of participants is one of the key metrics we strive to achieve. We naturally want our clinical trials to recruit participants who closely match the intended population who will benefit from the drug when it is eventually approved,” said iNGENū CEO Dr. Sud Agarwal.
While the inclusion of women in psychedelic clinical trials is critical to the success of this new paradigm in medicine, there’s also a whole realm of largely untapped research on the benefits of psychedelics for health conditions experienced only by women.
Felicity Pharma is a psychedelic biotech company focused on women’s health that’s secured a proprietary psilocybin-based drug for premenstrual dysphoric disorder (PMDD), a very severe form of premenstrual syndrome that affects up to 10 percent of women globally as well as postpartum depression.
Olivia Mannix, Felicity Pharma co-founder and CEO, said “We are passionate about transforming women’s healthcare. Women have been traditionally excluded from clinical trials because of hormonal fluctuations and general biological makeup. We are making a stand to develop female-focused therapeutics, where women will be the only patients used in trials.”
In this episode, Kyle interviews C.J. Spotswood, PMHNP-BC: author and board-certified psychiatric-mental health nurse practitioner currently enrolled in CIIS’ Psychedelic-Assisted Therapies and Research certificate program.
Spotswood has worked with Psychedelics Today, teaching masterclasses for our Vital and Navigating Psychedelics for Clinicians and Therapists courses, but this is his first appearance on the show. His first book, The Microdosing Guidebook: A Step-by-Step Manual to Improve Your Physical and Mental Health through Psychedelic Medicine came out last year, and we’re giving away three signed copies (US and Canada only). Click here to enter!
He talks about his introduction to psychedelics and his first patient immediately asking him about microdosing; why he changed his mind on microdosing and why he wrote his book; microdosing studies he’s most excited about; the terms: treatment-resistant depression, risk reduction, and flight nurses; Irving Kirsch’s work uncovering the bad science of research studies; the need for physicians to know enough about psychedelics to be able to meet their patients where they are; the importance of group work; and how, while they’re already so well-versed in caring for patients, using nurses to their full licensure could be the answer to the quickly growing psychedelics and scalability problem.
“When you look at the early research into the 50s in the 60s; they were doing microdosing research, they just didn’t have a title for it. They thought they were using placebo levels but they were actually looking for threshold levels; things like that. Really, it was what by today’s standards [would be an] amount that we would consider as a microdose.”
“I don’t like the term [treatment-resistant depression] when we use that because if you’re using [it] when you’re looking at the standard medications like SSRIs [or] SNRIs, they’re basically all the same. …So when you say that someone’s ‘treatment-resistant’ for three medications, four medications that are all basically working the same pathways and in the same amount; is that truly treatment-resistant, or are we just trying the same thing with just different medications, whereas doing microdosing is a different pathway [and] is a different approach?”
“My first patient I ever saw as a new clinician, like, literally my first patient: I come in and I’m starting to talk to them for the first interview and I got to the point and I’m asking them: ‘Where are we going, what do you need?’ and they said to me, ‘Do you know anything about microdosing?’ …I said to them, I go, ‘Yeah, I know a little bit.’ …So I asked her what she knew, and she knew quite a bit. And she goes, ‘What do you know?’ and I kind of just said to her: ‘I don’t really know how to put this, [but I] wrote a book on it and it’s going to be coming out next year.’ …It reinforced my feeling [that] I’m doing the right thing: this career suicide I’ve thought of, going into working with psychedelics and being open and talking about it, hearing my first patients talking about it – it’s got to be serendipity.”
Wmtw.com: ‘Zombie’ drug Spice worsening Maine epidemic, officials say
The Psychedelic Explorer’s Guide: Safe, Therapeutic, and Sacred Journeys, by James Fadiman, Ph.D.
Psychedelics Today: Surprising Results: Psilocybin Trial for Depression Alleviates Chronic Pain
Pubmed: Low doses of lysergic acid diethylamide (LSD) increase reward-related brain activity
Nature.com: The Discovery of Serotonin and its Role in Neuroscience
Psychedelics Today: PTSF89 – A Macro Dive Into Microdosing
Emperor’s New Drugs: Exploding the Antidepressant Myth, by Irving Kirsch, Ph.D.
In this episode, Joe interviews New York Times best-selling author, pioneer in the field of integrative medicine, and overall legend in the health and wellness space: Andrew Weil, M.D.
As the author of 15 books on health and wellbeing and a regular in the media, you’re probably familiar with Weil and some of his work, but you may not know of his more psychedelic connections: a long history of experimentation, leading Paul Stamets in the direction of functional mushrooms, co-writing one of the first papers about the Sonoran Desert toad and 5-MeO-DMT with Wade Davis, and being a strong advocate for psychedelics being the spark that could spur a global change in consciousness.
He talks about the connection between true osteopathy and integrative medicine; why the traditional Chinese medicine approach to mushrooms made so much sense to him; academia’s lost interest in pharmacognosy; how psychedelics may help people with autoimmune diseases; turmeric (he largely popularized it as an anti-inflammatory supplement); matcha; why we should be studying the placebo effect much more than we are; humanity’s innate drive to experience altered states of consciousness; and why a big part of the psychedelic revolution is so many people starting to believe in panpsychism.
We’re pumped to finally have him on the podcast, and we’re even more excited that he’s spreading the gospel of psychedelics to a health and wellness crowd who may still be a bit apprehensive about something they were taught to fear.
“I’m tremendously interested in [psychedelics’] potential at the moment for therapeutic use and ceremonial use, and actually, if I think about it, I would say I’m really interested in the possibility that they can save the world. I don’t see many other things out there that can do that.”
“I don’t know anything else that is so readily available and that, with at least some attention to how you do them, has such a potential to change how people interpret their perceptions and interpret their experience of the world around them. I’ve seen just such dramatic changes in people and in myself as a result of psychedelic experience. …My first book, The Natural Mind, that was published in 1972, said that only a global change in consciousness could really transform our world, and I think that the psychedelic revolution has the potential to do that.”
“I think the placebo response is the meat of medicine. That’s what you want to try to make happen. It’s pure healing response from within, mediated by the mind and unmixed up with the direct effects of treatment. …The commonest way I hear that word used is things like, ‘How do you know that’s not just the placebo response?’ or ‘We have to rule out the placebo response.’ I mean, we should be ruling it in. You want to make it happen more of the time.”
“Human beings have an innate drive to experience altered states of consciousness, not necessarily through the use of drugs (although drugs are a very convenient way to do it). One of the examples I gave was of kids learning to spin until they get dizzy and fall over and the world changed, and that’s universal as far as I can tell, in all cultures. So I got a lot of crap from people for saying that there was an innate drive toward altered states of consciousness, but I absolutely believe that, and I think that a part of the drug problem in our culture has been our failure to acknowledge that and teach people safe and better ways of satisfying it.”
The Andrew Weil Center for Integrative Medicine
Dr. Weil’s Matcha (use code: PsyToday for a generous discount!)
Wikipedia.org: Robert C. Fulford
Psychedelics Today: Wade Davis – Ayahuasca and a New Hope for Colombia
Psychedelics Today: Could the Sonoran Desert Toad Cure Narcissism?
Pubmed: Bufo alvarius: a potent hallucinogen of animal origin
Psychedelics Today: Dr. Malin Vedøy Uthaug – Ayahuasca and 5-MeO-DMT Research
Psychedelicreview.com: Psychedelics as Anti-Inflammatory Agents
Usnews.com: Is the Green Mediterranean Diet Healthier Than Regular Mediterranean?
Psychedelicmedicinecoalition.org
Vogue.com: Can Psilocybin Challenge Our Pharmaceutical Dependence?
From Chocolate to Morphine: Everything You Need to Know about Mind-Altering Drugs, by Andrew Weil
Psychedelics Today: PT236 – Drugs: Honesty, Responsibility, and Logic, featuring: Dr. Carl Hart
Psychedelics Today: Psychedelics, Philosophy, Transhumanism, and Peter Sjöstedt-H
Exploringyourmind.com: Panpsychism: A Fantastic Theory About Consciousness
In this week’s episode, Joe and David team up for the first time to discuss three articles: Chacruna’s breakdown of the study, “Ceremonial Ayahuasca in Amazonian Retreats – Mental Health and Epigenetic Outcomes From a Six-Month Naturalistic Study,” Double Blind’s “Why the ‘Psychedelic Renaissance’ is just Colonialism by Another Name,” and the results from the trial of a 20-year old woman who died at the 2017 Lightning in a Bottle music festival – where the jury found Do Lab, Inc., RGX Medical, and RGX Founder Richard Gottlieb to hold 75% of the liability in her death, with MAPS holding 25%.
In discussing these articles, much is covered: methylation and genetic memory; addiction; gut biome; cesarian births; how much inequality is built into the “psychedelic renaissance” due to it primarily evolving out of inherently unequal Western societal paradigms; permaculture; new ways to be together; Burning Man; the concept of the nuclear family; the power in working with your hands; creativity; harm reduction and the lack of readily available drug testing kits; and more.
Psychedelics Today: PT295 – Sidarta Ribeiro – Dreams, LSD, and Biopiracy
The Way of the Psychonaut Vol. 1: Encyclopedia for Inner Journeys, by Stanislav Grof, MD, Ph.D.
Doubleblindmag.com: Why the “Psychedelic Renaissance” is just Colonialism by Another Name
Wikipedia.org: Nagoya Protocol
How Soon Is Now?: A Handbook for Global Change, by Daniel Pinchbeck
Shop Class as Soulcraft: An Inquiry Into the Value of Work, by Matthew B. Crawford
Maps.org: Jury Finds in Favor of Plaintiffs in Trial on Harm Reduction and Medical Responsibility
Lucid.news: MAPS Found Liable in Wrongful Death Lawsuit
MAPS’ Settlement-and-Release-Agreement-5.27.21
In part 2 of the article, “Surprising Results: Psilocybin Trial for Depression Alleviates Chronic Pain,” the disappearance of Court’s chronic pain leads to a new understanding of cortical remapping, mirror box therapy, and how science can treat phantom limb pain.
I had years of experience in cold water training from my Aikido career, but as my depression had increasingly grown worse, I developed a severe cold intolerance. It had become painful to stand under the shower, with my scalp almost spasming in contraction, when I used to be able to stand in late winter melt-water waterfalls and rivers with ease. But post-dosing, my cold tolerance came roaring back; allowing me to stand under a cold shower for minutes at a time with no numbness and no pain – it was almost like it was happening to someone else or there was a micro-force field on the surface of my skin. I found myself having to leave the shower because I just had other things to do. Cold water tolerance is a gold-standard for measuring pain response in clinical trials, and in fact, later that year, the Department of Psychopharmacology at Maastricht University, sponsored by the Beckley Foundation, conducted the first LSD and pain study in nearly 50 years, showing that low-dose LSD significantly increased cold water tolerance without interfering with day-to-day activities.
I had been known for my mobility and flexibility throughout my career and my ability to train others to achieve the same results, but mine had been compromised for a good while at this point. But the day after my session, I was able to resume positions that I hadn’t been able to comfortably acquire in months, if not years. Movement now felt smooth and effortless once again, and I swear there was even improvement in the tissue quality in areas that had become “crunchy.”
There was also a significant change in my inflammatory baseline. Depression is seen as a disorder that also includes fairly significant neurological inflammation and is often bi-directional with chronic pain, but many of the same receptors that psilocybin operates on are also contained within the gastrointestinal tract, and mine had altered sensation for a month afterward. I believe my systemic inflammation significantly improved during that period because within three months of my dosing, I reacquired personal training records that had become elusive, and by summer, I passed those PRs and set new ones. I also felt incredibly less “puffy.” Accidentally banging into something didn’t hurt anymore and persistent joint aches and lack of motor activation disappeared. There were additional improvements in neurological issues that will be described in a future case study, but that was just as immediate and impactful.
Within the training and recovery world, patients and trainees can loosely be categorized as super, normal, non, and negative responders. I had stopped being responsive to both training and rehabilitation efforts at the peak of my depression, and was entering negative-responder territory, which was severely distressing. Fascinatingly, I now seem to be trending somewhere between a normal and high responder. I began proclaiming to the researchers at NYU that psychedelics were going to completely change chronic pain treatment within five years. And I also had a secret; the day after my dosing session, I had what’s referred to as a huge download: I realized that if you could consider things like depression, PTSD, and severe anxiety to be nociplastic outputs of the Central Nervous System (CNS) that causes iterative rumination (a.k.a. looping maladaptive outputs), that was no different from the looping maladaptive outputs that characterize chronic pain – the neurology of which I had been studying for years at that point. Due to the extreme visual qualities of the psychedelic experience and the rapidity of my own remission, I saw, in a flash, that since psilocybin was an impact booster for neuroplasticity, it would enhance the impact of mirror box therapy for phantom limb pain or likely any other neuromodulation.
“Remapping” is the term describing the tactic of using visual or other sensory receptor inputs to modify and change nociplastic or noxious/painful outputs of the brain. As this is part of the Z-Health process, I had been introduced to the concept of mirror box therapy years earlier as part of my certifications, but I thought I had come up with a whole new approach and kept it to myself, barely hinting at what I believed I had uncovered. But, since NYC was locked down and I was unable to work, I had nothing to do but go online and research what had happened to me.
Within two weeks or so, I found an old photocopied English abstract from a 1962 study in Japan, by Kuromaru, et al., using low-dose LSD to treat phantom-limb pain with 50% of its participants going into instant remission by the end of their session, and the authors pointedly declaring that stacking the LSD with movement had a far stronger impact on resolving both phantom limb pain and phantom limb syndrome. Stacking inputs is a common practice within the neuromodulation world for pain treatment, often coupling a weaker input with a stronger one, and I realized that this was what had clearly happened to me while I was in my post-dosing neuroplastic window. It finally felt like I was getting traction again; that drills and exercises were once again effective, and crucially, maintaining their own momentum. I didn’t have to be hypervigilant anymore in my daily routine for these drills to become “sticky.” I also realized that the Kuromaru study had, in fact, been released earlier than the Kast study from 1964 investigating the analgesic properties of LSD for terminal cancer and other painful conditions, which is frequently and incorrectly cited as the first psychedelic pain study. I became aware of other previous psychedelic pain studies, as well as recent ones like Dr. Charles Nichols’ work on the anti-inflammatory properties of psychedelics, and studies involving Dr. Robin Carhart-Harris’ REBUS model and cortical reorganization, which is what happens when a stimulus results in the creation of a new cortical map (essentially a vertical column in the brain cortex consisting of neurons performing specific processes).
Both of these discoveries are crucial because cortical reorganization (or remapping) and inflammation are key drivers of chronic pain. Conditions like depression and anxiety are characterized by rigid, fixed beliefs or frameworks where the same negative thought loop keeps reoccurring repeatedly, with no amount of incoming contrary information able to alter that belief. It becomes what’s known as a “strong prior” in neurology, becoming a top-down driven process in the CNS, actively suppressing any bottom-up sensory input error correction. The same mechanisms of action occur with chronic pain, where, despite the healing or resolution of an injury; a rigid, fixed pain signal is continually being sent out by the brain as a maladaptive response of the CNS’ protective suite. These are referred to as nociplastic or noxious neurological conditions. The same is true for multiple chronic pain conditions where inflammation causes maladaptive signaling and perceptions, leading to negative structural or nociplastic changes in the peripheral and central nervous system. In psychedelic-assisted psychotherapy, a non-rigid, chaotic state is induced, which allows the cortical landscape to reorganize into a more efficient and positive state.
As everything was becoming more and more clear – in what had to have been one of my most transpersonal moments after my dosing session – a landmark review paper was published. “Chronic pain and psychedelics: a review and proposed mechanism of action” by Dr. Joel Castellanos, et al. was released from the Psychedelics Health and Research Initiative (PHRI) at UC San Diego in May of 2020, barely two months after my dosing session and pain revelation. It was an amazing overview of all the possible mechanisms of action that could be at play in psychedelics being an effective analgesic and resolver of chronic pain, but the most revelatory moment was when I found, buried within the heart of the paper, a link to the case study that had set PHRI in motion. It was written by the world-renown neuroscientist VS Ramachandran, the clinical faculty at PHRI, and by its case subject, Albert Lin, who had used high-dose psilocybin coupled with mirror box therapy to put his intractable phantom limb pain into full remission.
I sat speechless for at least five minutes, shaking my head in a feeling of wonder and disbelief, as if the universe itself had just delivered this paper to me. Other than my remission and the pandemic, I had thought of nothing else but the application of how these two approaches could be combined. Of course someone else had invented it well before me; of course they had. I knew that resourceful, capable people had been working on this for a while, and chronic pain is a singular motivator, but it was still astonishing to see my vision so vividly applied and executed.
I had learned in 2015 that cluster headaches had been effectively treated with psilocybin for 25 years, and of mirror box therapy a few years before that. I had even blogged about it because people in the rehab and training communities thought that my using visual inputs to treat pain was so weird they called it “voodoo.” But there is a neural hierarchy, and many pain and performance conditions in the body actually have higher-order components within the visual and vestibular systems. That’s often why, no matter how much manual/physio therapy one does, it is often a downstream compensation within the body in order to reconcile perceptual discrepancies between the visual and vestibular system. The visual system lets you assess the surrounding environment and predict any threats that exist within it, and the vestibular system helps you orient within that space, keeping your body in balance so that you might be able to execute any motor actions in response to any perceived threats. If your eyes are telling you the horizon is 5° tilted to the left, but your vestibular system, a.k.a. your inner ear, is telling you that it’s 5° to the right, your body will compensate so that those discrepancies are reconciled and you maintain a stable, level “sight picture” – your viewscreen of the world. Having an unstable sight picture makes for poor predictions; in other words, in an evolutionary survival context, having a “shaky cam” is not so great for avoiding saber-tooth tigers.
So, those downstream bodily compensations that keep your viewscreen steady are creating distortions and possible maladaptations in the structure of your body, and are now being cemented due to repeated compensatory use. The nervous system will protectively reduce motor output and increase pain perception as a response, to slow you down in order to avoid potential injury and survive another day. Ultimately, the body has evolved towards survival, not performance. And pain is an alarm/action signal designed to keep you alive.
When we look at phantom limb pain, what we’re seeing is the phenomenon known as deafferentation: the loss of afferent or ascending inputs from the peripheral nervous system up to the brain. No limb equals no signal, and the loss of signal is very dangerous within an evolutionary context because limb loss due to injury or infection will mean, at the least, loss of sensation and loss of coordination for motor outputs/muscle contraction/movement, meaning a lost ability to gather food or to avoid threats. Or worse, it could mean signaling that you’re going to bleed to death in a matter of minutes.
Multiple pain conditions could be considered sub-clinical deafferentation: peripheral neuropathy from conditions like diabetes or shingles, or different types of phantom limb pain where the limb is still present but the nerves are so injured that they no longer transmit afferent signals – such as we see in cancer, stroke, or crush injuries. That loss of signal gets hardwired into the cortical representations of that limb, and never gets a counterbalancing signal, so the CNS registers it as an ongoing sense of threat. That creates a huge alarm signal in the form of pain perception.
What mirror box therapy does is replace that loss of signal with the image of an intact limb, generating input that dampens down that pain signal. And when you touch the remaining limb (which is generating normal signals) while seeing it reflected in the mirror in place of the missing or injured limb, it can immediately cause the pain signals to cease; so powerful are visual representations within the somatosensory cortex of the brain. Essentially, through seeing a limb appear where it wasn’t before, one tricks their own brain into thinking it’s still there, and the pain signals from the CNS for that lost limb stop being sent.
Mirror box therapy is often not enduring though; only being effective for as long as you do it, and that was the case with Albert Lin. It often takes a lot of repetition for it to become “sticky.” Neuroplasticity requires novelty and intensity, usually in the volume of work. But that can be hard to achieve, thus the issue in pain treatment that I had experienced directly as a practitioner and as a patient; everything works, nothing lasts. When it was suggested to Lin that psilocybin had strong neuroplastic properties that could impact cortical reorganization for chronic pain, he tried it a few times, taking a high dose of psilocybin mushrooms, which gave him approximately 3-12 pain-free hours, depending on the dose. But then the pain came back with a vengeance. Within the cluster headache communities, this is known as a “slapback effect” and can actually be a sign that the nervous system is adjusting and more permanent relief could be imminent.
Then, Lin’s wife suggested combining (stacking) mirror box therapy with psilocybin. He went out to the desert with a closet door mirror, and while under high-dose psilocybin, he would stare at the reflected image of his remaining leg and then at the space where his amputated limb had been, while repeating the phrase “You are safe. You are totally safe,” for approximately 45 minutes. This met all the conditions for driving neuroplasticity: novelty, intensity, and volume of work with deep assurance of emotional and physical security. Amazingly, it worked, immediately putting him into remission for the next 20+ hours, with 50% reduced pain for nearly two weeks. He shared his success with the lab, and experiments with different types of visual neuromodulation while under high-dose psilocybin quickly began.
Lin was dealing with a persistent pain in his phantom foot that felt as if a railroad spike was being driven through, suspected to be a sensory remnant from when the bones in his foot were surgically pinned together as they attempted to save it before ultimately deciding to amputate. An artificial foot and a pen with a telescoping pointer was introduced, and they covered the space between his stump and the plastic foot with a blanket, then “pulled” the telescoping pen out of his foot at the site of pain, mimicking the action of removing pins (or really, removing the pain). He felt instant relief.
Another experiment involved a novelty Halloween-store “flame” (bright light with orange and yellow fabric and a fan underneath that makes it flutter). Lin chuckled when he saw it, but when they brought it near his representational foot, he actually felt heat from the “flame,” which was intensely relieving.
Through these experiments and continued work, Lin went into full remission after five weeks, and has been free of chronic pain ever since. It’s worth noting that he had a top research team working with him that was extremely creative in creating novel inputs, and he is known for being an almost Michelangelo-type character, with a high degree of inventiveness and novelty-seeking, allowing him to discover unique, lateral approaches to solve problems. And, it bears repeating: chronic pain is a singular motivational force.
Additionally, post-dosing, cortical reorganization was happening during a psychedelically-induced “critical period reopening”; when the brain has a metaplastic quality that allows it to reset to an almost-new condition. As described in the work by Dr. Gül Dölen, critical period reopening happens during crucial phases of nervous system development in childhood, such as when toddlers can learn multiple languages without an accent or when adolescents are uniquely sensitive to social cues from peer pressure (and/or support), allowing them to quickly adopt different social customs and frameworks. This reopening is also seen post-stroke, when there is a limited window for rehabilitating from brain injury, so this likely applies very well here with chronic pain. We know that veteran groups like the Heroic Hearts Project, VETS (Veterans Exploring Treatment Solutions), and The Mission Within, who are employing psychedelics for treatment, are having striking results both in recovery from combat-induced PTSD as well as traumatic brain injury – typically seen as treatment-resistant conditions.
If there’s anything I would like you to understand after reading this article, it’s that:
We don’t have to prove that psychedelics are effective for treating chronic pain; we have to establish that this has already been proven.
Psychedelics are not an instant cure for chronic pain, but they are strong impact boosters for neuroplasticity and can make physiotherapy/neuromodulation become “sticky,” creating enduring relief.
We know that many mechanisms that create psychiatric conditions that are responsive to psychedelic-assisted psychotherapy are extremely similar in nature to the same mechanisms that generate chronic pain; it’s just that psychiatric conditions have gotten far more focus in psychedelics, perhaps because the non-ordinary states of consciousness they are known for producing seem more applicable to conditions more traditionally thought to be related to the mind.
But both arise out of the central nervous system and are rigid, fixed states of cognition and perception. With depression, you have negative outlooks and self-perceptions: “Nothing I do makes a difference,” “People are just saying that to make me feel better,” etc. At one point, these thoughts may have helped you to cope with a traumatic incident, environment, or upbringing, but now they’re maladaptive, weigh you down, are out of step with reality, and have actually caused (or are the result of) structural deficits in the neurology of your brain. It’s the same with chronic pain: when there is an acute injury or even the possibility of one, pain is part of the protective suite of responses from our nervous systems to prevent further injury and allow healing to occur – an alarm bell/action signal to change a behavior. But it can be so overprotective that it gets embedded and cemented with movement, emotions, and surrounding environments long after all tissue healing is done – getting triggered by seemingly innocuous events, maladaptively hardwired into your neurology in a negative loop of conditioned responses.
This is exactly what happened to me when I went through NYU’s psilocybin trial; an adverse financial and work environment, repeated (and under-recovered) musculoskeletal stress/injuries, and (likely) sub-clinical post-concussion syndrome and PTSD, all topped off by the sudden death of a close friend releasing long-suppressed grief and leading to a significant nociplastic output in the form of increasingly treatment-resistant depression and moderate chronic pain. Many recovery efforts were attempted using every modality I knew, but there was too much of a deficit to overcome – until psilocybin was introduced to the mix. That life-changing experience allowed for metaplasticity, cortical reorganization, descending inhibition, and anti-inflammatory properties to take root, giving all post-dosing interventions the opportunity to gain traction and for me to flourish once again.
Future articles in this “Pain and Psychedelics” series will focus on old assumptions vs. new science, additional case studies, the suspected mechanisms of action behind the interaction between psychedelics and pain, and best practices and safety concerns for working with psychedelics to alleviate chronic pain.
An NYU psilocybin depression study participant discovers an unforeseen application for psychedelics: the treatment of chronic pain. Part 1 of the series: Psychedelics and Chronic Pain.
In the fall of 2020, I was living a pretty successful and happy life – on paper. I had co-founded a very popular, leading-edge CrossFit gym in NYC; one of the first in the world. I held multiple advanced certifications in applied neurophysiology through Z-Health, helping clients with challenging pain and performance issues. As an early adopter of kettlebell training, I became a nationally top-reviewed instructor and trained Team 6 Navy SEALs, astronauts, pro athletes, wounded veterans, and members of the FBI, NYPD, NYFD, and ROTC. I was featured in Men’s Fitness, the NY Times Sunday Routine, and USA Today. I had 30 years in the pain & performance field, training and teaching at a high level, and was becoming widely known for helping people with difficult mobility problems or chronic pain, using unique methods from the leading edge of neurological rehabilitation. On top of all of that, I was 17 years sober.
However, not all that glitters is gold. A now ex-business partner was committing a Ponzi scheme to the tune of millions, and his case followed him like a shadow, turning my life’s passion into an emotionally and financially toxic nightmare that economically devastated my family. My best friend, Kirk MacLeod, who I had completely rehabbed from chemo & cancer surgery, died six months after being declared in remission. My first son had developed undiagnosed GERD and couldn’t sleep more than an hour and half at a time, which meant my wife and I slept even less.
Unsurprisingly, my episodic depression returned after more than a decade and a half, and I was now increasingly treatment-resistant; unresponsive to psychiatric drugs that had previously worked. All my pain neuromodulation interventions that worked on my clients no longer worked for me, and I had developed chronic pain myself.
I share all my background here to demonstrate that I was not under-resourced in either knowledge, networks, or diversity of approaches, practice, or experiences. I poured over all my certification materials looking for anything I had missed, but had fallen into an increasingly deeper recovery hole; everything worked, but nothing lasted. I was hitting a new bottom in my life, deeply sinking into the midst of an increasingly treatment-resistant depression episode that had likely been ongoing for five years.

But then I became aware of ongoing studies on psilocybin for depression happening locally in NYC. I had experienced a few high-dose psychedelic sessions nearly a quarter century ago and had been an avid Terence McKenna fan (even speaking with him directly after a lecture in Seattle), but I had never taken psychedelics therapeutically, and my recreational interest had effectively vanished once I became sober from alcohol. Intrigued, I connected with the local clinical research coordinator, Leila Ghazhal, at the NYU for the clinical trial of Psilocybin for Major Depressive Disorder study (sponsored by the Usona Institute), and took all the online and over-the-phone assessments, passing them easily. The primary investigator (PI) on my study was Dr. Stephen Ross, who had been leading psychedelic research at NYU for more than a decade. Amazingly, I made it into the trial within a month and a half, learning that I’d actually beat out 8500 other applicants for just 100 spots nationwide.
When I first entered the trial, I was in a state of denial about how severe my depression was, but once I took the MADRS assessment, there was no avoiding that I had moderate to severe depression with suicidal ideation.
I remember a specific moment very well during this process, when I was finally cleared to enter the study and the study coordinator was speaking with me about the results of my assessment and my upcoming participation. I asked what would happen if I didn’t receive psilocybin during my session, and he reassured me that they would not just drop me off in the middle of the ocean to dog paddle – that there were other interventions and studies available and they would be sure to find me something, but there was a good chance I would receive psilocybin and hopefully get some good results. At this point, my mask cracked a little bit and some protective cynicism came out, and I quipped with a bit of a shrug: “Well, we’ll see.” I hadn’t meant it to be dismissive or sarcastic but it came out that way, and the conversational atmosphere rapidly shifted. He looked right at me and suddenly he wasn’t the primary investigator anymore, lost in the myriad details and logistics of a very involved study. Now he was the deeply experienced clinician and therapist, and, having heard something within the tone of my voice, dropped all the way in and asked softly: “What’s going on behind that, Court?” Suddenly, all the masking dropped and there was no more place to hide because I was so, so tired at this point, and had been waiting for this moment. In and out of therapy for years, dozens if not 100 self-help books, so many modalities, so many somatic systems, and here I was with a chance for something new to help me. When I realized why there was cynicism behind my statement, my voice cracked, I started crying, and I answered him: “Trying not to hope.”
The one glimmer of hope I did have was reading a 2018 paper by lead author Calvin Ly describing psychedelics’ neuroplastic activity in the prefrontal cortex. As someone who had studied the neurology of pain for years, this was revelatory. Many pain conditions are, in fact, nociplastic or noxious conditions arising out of the central nervous system (CNS); there’s no more injury or damage if there ever was, but your CNS is still continuing to put out a maladaptive alarm signal that is perceived as pain. So learning that psilocybin was creating actual structural change within my cortex – not “just” psychological change – was completely astonishing.
My dosing date was on March 5, 2020, and I remember looking down at the capsule sitting in the cup, saying to it: “I really hope that’s you.” I was terrified inwardly that I would receive the placebo, that I wouldn’t respond to the psilocybin, or that it would only work just a little bit, only for its effects to slowly fade. But within half an hour, there was no denying that I had received psilocybin, and I earnestly pursued all the procedures everyone on my care team at NYU had worked with me on for weeks in preparation for this day.
I was genuinely shocked at the sheer volume of psychological material from my childhood and early adulthood that came up. I had profound transpersonal experiences and healing, revisiting instances that were pivotal in my childhood. I had an encounter with the first woman I had ever loved, who had committed suicide three years after we had broken up. Her death had caused a profound grief in me that drove my drinking for a decade after. I thought I had released the majority of my grief around her once I got sober, but clearly, there was so much more to heal that had been deeply suppressed as I tried to move forward with my life.
The biggest shock of all, though, was waiting for me at the end of the day when one of my facilitators casually pitched a seemingly routine question while closely watching me out of the corner of his eye: “So, how do you feel?” Without thinking, I reflexively replied, “Good,” but then, just as reflexively, scanned more deeply inward, and in a sudden rush, realized my depression was completely gone – not just better, but vanquished, exclaiming: “Good! That fast? Are you fucking kidding me, that fast? Is it gone already?”
It felt as if a huge mass had been surgically removed from me or as if an entire continent within my interior was now suddenly revealed. No matter how many times you read the word “remission” and the percentages behind it in scientific studies, very little will prepare you for the shocking reality of it. The contrast between before and after was profound. All of the iterative rumination was gone, and it took no effort for that to happen. And it only seemed to strengthen as the days passed. Miraculously, all suicidal thoughts ceased on that day and never returned.
Shockingly, only ten days after my dosing session, NYC went into a complete pandemic lockdown, my entire industry closed, and my two young boys were now at home with me 24/7, tele-learning. I cannot imagine what 2020 would have been like for me if I had received the placebo. It’s almost unimaginable.
But here is where the story takes an even more profound and impactful turn. During the session, my leg started intensely tremoring/spasming. I had been evaluated for musculoskeletal pain and dysfunction that I had acquired through a host of injuries over the years of my performance career, and in fact, had just been in the doctor’s office a few months earlier trying to determine if I had arthritis or something worse. But right there in the session room, I started having a neurological revision, with my muscles and nerves in my right inner thigh firing in an effort to recalibrate the sensory and motor inputs and outputs in that part of my kinetic chain. It was almost like a self-generated TENS unit (Transdermal Electromagnetic Nerve Stimulation, used to generate muscle contractions and neuromodulate pain signals with micro-electric pulses) getting my leg back online by creating intense motor activity in the muscles of my thigh.
I’ve since spoken with spinal injury survivor Jim Harris and read a case series from UC San Diego’s Psychedelics and Health Research Initiative (PHRI) published in PAIN Journal where the exact same thing occurred to them under the effect of psilocybin with the same positive results, but at the time, the facilitators were concerned enough to ask the primary investigator to come and evaluate me during the session. I had to explain to him, somewhat hilariously as I was going into my peak, that, in fact, the tremors felt intensely good. I’m grateful that he let them continue because it has made all the difference.
While I partially understood what had happened, I was understandably beyond eager to learn more, and to see where else this realization could take me: Why did this work so well? Has our understanding of chronic pain been wrong? And if psychedelics are the answer, what does treating chronic pain with psychedelics actually look like?
This is part 1 of a 2-part piece and part of a larger series on chronic pain and psychedelics. In part 2, I will dive into the research around remapping and mirror box therapy, and why my psychedelic experience seemed to be so effective.
Future articles will focus on: What is pain and what causes chronic pain, old assumptions vs. new science, the suspected mechanisms of action behind the interaction between psychedelics and pain, and best practices and safety concerns for working with psychedelics to alleviate chronic pain.
In this episode, David interviews Dr. Ben Medrano: Co-Medical Director with Nue Life, board-certified psychiatrist specializing in integrative psychiatry, and former Senior Vice President and US Medical Director of Field Trip Health.
He discusses his path to Nue Life; from growing up around mental illness, to the rave scene, to Buddhism, to his years working for the underserved in an East Harlem Assertive Community Treatment, and his biggest takeaway from that time: that the healthcare system he knew was not truly helping people. He talks about stigmatization (of some modalities like electro-shock treatment, of psychedelics, and of ketamine – which seems to be stigmatized even within the psychedelic space); his concerns that the at-home ketamine model is at risk as we make our way out of the pandemic; and how at-home ketamine can drastically reduce the cost of treatment.
Medrano tells a great story of a patient who saw incredible improvements through ketamine, and discusses some Nue Life highlights: their just-released 664 participant-study in Frontiers Psychiatry showing the safety of at-home ketamine (and that at-home is just as effective as other routes of administration); Nue Care, their model for aftercare using digital phenotyping, goals, and a scoring system (which he believes could be the new model for integrative psychiatry); and their Nue Network, which could be a solution for better education on ketamine and for granting access for patients through prescribers who typically don’t understand much about its efficacy.
“All the different interests, personalities, visions, [and] goals that are in this sort of circus of psychedelic commercialism is very necessary to understand. And for me, I think the biggest takeaway is that there is one thing that binds everybody who’s involved, and that is hope, really. I think there’s a lot of hope in this sphere.”
“The hazards of a benzodiazepine are well known, and to some extent, one might even argue that with some of these DEA-regulated substances that we do ship at home; that if we’re going to say that we need to subject ketamine to a higher standard, then we need to do it for the rest of these DEA-regulated substances, because they have very hazardous risk profiles. …I can’t help but think that there’s a little bit of …stigma [around] what it is that we’re doing.”
[On an at-home ketamine patient’s success]: “He is able to get out of the house every day and enjoy the sunshine, and the way he views his trauma is at a level that I think all of us would aspire to: really, as something that has sort of made him into the man that he is today, with something really unique and powerful to offer as a human to others – rather than as a wound.”
Psychedelics Today: Free Webinar – NueLife: Empowering Patients with At-Home Ketamine Therapy
Wikipedia.org: Assertive community treatment
Legitscript.com: A Post-Pandemic Ryan Haight Act May Create Uncertainty for Telemedicine
Nue.life: Nue Life Publishes First Peer-Reviewed Study in Frontiers in Psychiatry
In this episode, Joe invites Court Wing to co-host, interviewing two members of UC San Diego’s Psychedelics and Health Research Initiative (PHRI): Joel Castellanos, MD (Associate Medical Director of PHRI and board-certified physical medicine and rehabilitation and pain medicine physician), and Timothy Furnish, MD (Medical Director of PHRI and Associate Clinical Professor of Anesthesiology and Pain Medicine).
As one of the early participants of a psilocybin-for-depression trial in NYC, Court Wing (of REMAP Therapeutics) discovered that immediately after the session, his chronic pain had miraculously gone away. He began researching how psychedelics could be used (with or without other therapies) to continue the alleviation of pain psychedelics had brought him. Through the Psychedelics and Health Research Initiative, Drs. Castellanos and Furnish are following that that same road, and are currently recruiting for a randomized controlled trial on psilocybin for phantom limb pain.
They talk about the relationship between the mind and chronic pain: how people confuse pain with the simple act of nerves firing, but how it’s so much more. And they discuss how pain can become part of one’s identity (and how the Default Mode Network could be contributing); how physical therapy is related to neuroplasticity; mirror box therapy; microdosing for chronic pain; the unusual nature of phantom limb pain; and where the mystical psychedelic experience may come into play. If this topic is as fascinating to you as it is to us, stay tuned – we will be featuring much more on chronic pain and psychedelics, including a blog series from Court Wing coming soon.
“One of the things that may be unique about or interesting about chronic pain is that the longer it goes on, the more people start seeing pain as a part of their identity and that Default Mode Network is probably playing a role in that. And it’s possible that something like psychedelics could open up the possibility of changing that internal story so that pain is no longer so much a part of one’s identity.” -Tim
“I think that people oftentimes confuse pain with simply nerves firing. …[But] there is this rich interplay between the way we think about pain, the way we perceive pain, and how we feel about it.” -Tim
“When you’re not really dealing with chronic or severe pain on a daily basis, it’s really hard to think about how life-changing that is or can be.” -Joel
“When we hear things like ‘It’s only just in your head,’ I don’t think people quite get [that] the head can be a scary place to be trapped sometimes.” -Court
PHRI.ucsd.edu: Psychedelics and Health Research Initiative at UC San Diego
Psychedelics Today: Court Wing – Pain and Its Relationship to the Mind
Pubmed: Chronic pain and psychedelics: a review and proposed mechanism of action
Sciencedirect.com: Mirror Visual Feedback Therapy. A Practical Approach
Psychologytoday.com: Catastrophizing
Physio-pedia.com: Kinesiophobia
Sinobiological.com: What is tumor necrosis factor (TNF)
Neuropathycure.org: Cryoneurolysis: A Freezing Cold Way To Treat Chronic Nerve Pain
Journals.lww.com: Microdosing psilocybin for chronic pain: a case series
Healthgrades.com: Diagnosing and Treating Anhedonia: Loss of Pleasure Explained
In this episode, Kyle interviews Dr. Steven Radowitz: Medical Director at Nushama, a wellness center in New York City primarily offering IV ketamine, with a strong focus on letting the experiencer explore their journey undisturbed.
Recorded in-person at Nushama’s flagship location just over a year after opening, Radowitz talks about his past and why he became interested in ketamine, the look and feel of Nushama, their process, and why they favor IV ketamine. He highlights his biggest takeaways from the year: the surprise in just how effective ketamine has been; the role of integration and what aftercare truly looks like; and the importance of learning to hold space and be a compassionate listener – that the doctor isn’t the healer and the psychedelic isn’t the magic bullet cure; instead, they are just tools that allow the patients to heal themselves.
He discusses how he sees psychedelics as a dimmer switch for the ego; how disorders are tools to deal with trauma; why he is reframing trauma as a learning experience; why he thinks ketamine will survive once psilocybin and MDMA are legal; why group work is so effective and powerful (and likely the new model for psychedelic therapy); and the importance of staying humble through all of this – humble to the power of the medicine and humble to the amazing capacity for people to heal and grow, simply by being allowed to explore their journey and be heard.
“I’m not a healer, and I often tell people [that] during their preparation, when I do my medical intake. I talk to them about that. I say, ‘I’m not here [to heal you], I’m here just giving you a tool. You’re the healer. All this stuff does is [that it] just takes away what’s blocking you from realizing that. It’s like a dimmer switch on the ego [and] on the mind.”
“I’m trying to move away from the word ‘trauma.’ It’s a difficult life event that’s there to teach us. It’s there for something. And with every one of those events; there’s a little jewel within it, but you have to go in there and go through it. And it’s just a cloud, just a myst, almost, that’s preventing you. Just push [through it] and hold space. As long as people are in a safe place to go there and journey there, then they’ll realize that it’s just an event. It’s just an experience, and you move on. That wisdom is: a memory without the emotion.”
“I think any type of journey work, any type of psychedelic work, I almost think you have to be called to it in a way. You shouldn’t be coerced, ever, into this. …I find that the ones that are really ready to do the work are finding us on our own.”


Could a nation defined by inflammation find relief in psychedelics?
It’s a verifiable truth that the United States of America may be considered a global leader, especially when it comes to the prevalence of mental and physical health disorders. In fact, of the nearly 330 million people in the population, millions to hundreds of millions of Americans suffer from chronic conditions like:
These sobering statistics beg the questions: How could a single nation of relatively modest size be home to such a vast selection of chronic diseases? And how could psychedelics be used to combat these conditions affecting so much of the population?
The answer begins with key lifestyle factors such as diet, exercise, tobacco use, or genetic predispositions, each of which contribute to the pathology of a given disease. For example, a 2010 study by the American Cancer Association found that 90% of Americans don’t meet their daily recommended requirement of vegetables, with 75% failing to eat even a single piece of fruit during an average day.
The American diet overall is egregiously devoid of whole grains, beans, fruits, vegetables, and nuts, with the US Department of Agriculture estimating they represent a mere 11% of the populous’ typical daily food intake. Despite this lack of prevalence, these unprocessed natural foods are otherwise rich in medicinal phytochemicals found to support the immune system and strengthen the body’s resistance to infections, as well as fight cancer and diabetes; diseases that are twice as prevalent in the US relative to the global average. Shockingly, the US also leads the world in obesity rates by nearly 400%, and is first in global consumption of sugar, outranking Germany by about 26% yearly.

Although diet quality is proven to significantly impact the likelihood of disease development, what Americans eat is only one contributing factor among many. Poor diet alone doesn’t explain the exceptional amount of chronic health conditions seen in the population. In fact, it’s estimated that over 60% of Americans suffer from at least one chronic health condition, 42% of the population are diagnosed with at least two, and up to 12% of Americans live with five or more chronic diseases.
To put those percentages in perspective, the 2020 election saw the highest voter turnout in 120 years, with the most votes for a single presidential candidate ever recorded in American history. Joe Biden reportedly received over 81 million popular votes, representing less than half of the 198 million Americans suffering from at least one chronic health condition, and only marginally more than half of the 139 million with at least two.
Despite the fact that they’re by no means a minority in the population, chronic diseases are found to disproportionately affect socioeconomic minorities in the United States of America and beyond. A recent study published in the journal, “Archives of Public Health,” used 20 years (1995-2015) of empirical data from the Organization for Economic Cooperation and Development (OECD) to investigate the impact of education on health across the populations of 26 countries, including the United States, Canada, United Kingdom, France, Germany, and other founding nations that became members when OECD was created in 1960. This data, taken from millions of people in numerous countries across the globe over one fifth of a century, clearly demonstrated that higher educational attainment in adults positively correlates with longer lifespans, better health outcomes, increased Gross Domestic Product (GDP) per capita, and reduced infant mortality rates.
Put simply, the OECD data suggests that highly educated adults with ample finances generally live up to 12% longer (8-10 years), enjoy healthier lives, make more money, and are less likely to die at birth or of cancer, when directly compared to individuals of lower socioeconomic status (SES). Unsurprisingly, adults with higher GDP per capita also spent more money on healthcare and education over their lifetime, with college and university education found to positively influence life expectancy, child vaccination, and enrollment of children in education, as well as negatively impact infant mortality. Taken as a whole, the OECD data demonstrates an essential principle:
If appropriate education and adequate income significantly increase life expectancy, then access to quality schooling, sustainable employment, and equitable socioeconomic mobility are inherent to health care services.
However, even if we factor in education and employment as essential contributors to health, the fact remains that as of 2021, over 85 million Americans older than 25 had attained a Bachelor’s Degree or higher, and US unemployment was a mere 3.7% in August 2022. Since neither education nor employment are able to fully reconcile the disproportionately large number of Americans currently suffering from chronic health conditions, there must be a deeper underlying cause contributing to the pathology of diseases reportedly observed in the country’s citizens and resident aliens.
Compellingly, inflammation has been identified as a central contributor to all aforementioned chronic health conditions and beyond, and is implicated in over 60% of all human deaths around the globe. Some may already be familiar with acute inflammation in the form of localized pain, redness and swelling, usually in response to an injury or infection. Acute inflammation is typically a normal immune response during which the immune system is activated through the release of specific proteins, essentially called inflammatory markers. These markers then act as beacons to recruit immune cells, which subsequently migrate to the particular body part(s) in need of defense or repair.
In contrast, chronic inflammation is less apparent and far less immediate, but has insidiously dire consequences when left unchecked. Instead of causing localized pain or swelling, chronic inflammation causes systemic issues with immune cell signaling through excess “noise” created by high levels of inflammatory markers. Rather than being recruited to areas of the body most in need of healing, immune cells are drowned in an overwhelming number of biochemical beacons and ultimately disoriented. By disrupting this essential communication between immune cells, chronic inflammation prevents the appropriate direction of immune cells to critical issues needing attention, and may instead direct disproportionate amounts of immune activity to arbitrary areas – thus crippling the body’s capacity to effectively heal itself or prevent systemic disease.
The dysregulation of the immune system may ultimately induce the development of one or a combination of diseases, including autoimmune disorders like Crohn’s Disease, IBS, Alzheimer’s, arthritis, and diabetes, as well as various cancers and neurological disorders. Furthermore, children of mothers with chronic inflammatory conditions are demonstratively more likely to be diagnosed with ADHD, anxiety, depression, obsessive compulsive disorder (OCD) and autism, especially when chronic prenatal exposure to maternal inflammatory markers is exacerbated by psychological or physiological stress.
Over the past 20 years, a growing body of research has further investigated the complex relationship between chronic inflammation, various mental and physical diseases, and socioeconomic status (SES). High levels of inflammation measured by markers in the blood of low SES patients were found to prospectively predict whether they would suffer from depression, heart disease, ischemic stroke, and/or mortality.
Furthermore, factors such as poverty, lack of social or educational resources, obesity, and diets rich in refined sugar were all closely associated with increased inflammatory markers, chronic diseases, and mortality rates. Stress derived from socio-political, financial, environmental (chemical, biological, electromagnetic), or psychosocial (relationship experiences, trauma, social conditioning) aspects of a patient’s life also reportedly influenced inflammation, with chronic psychological and emotional stress inducing a significant increase in observed blood inflammatory markers; thus promoting immune dysfunction and ultimately increasing the likelihood of chronic diseases in individuals of low SES.
Despite these undeniable correlations and profound implications, the medical model of inflammation as the root of disease is not a new concept. Whether willow bark or aspirin, both traditional Ayurvedic and modern Western medicine employ preparations of anti-inflammatory drugs to treat a number of maladies, from headaches to heart disease. In fact, many over-the-counter (OTC) medications, commonly prescribed pharmaceuticals, and even psychedelic drugs owe some portion of their medicinal benefits to anti-inflammatory effects exerted in particular tissues of the human body.
For example, recent research has revealed that two of the most commonly prescribed classes of antidepressants, Selective Serotonin Reuptake Inhibitors (SSRIs) and Selective Norepinephrine Reuptake Inhibitors (SNRIs), may instead induce their expected medical effect via anti-inflammatory action within the brain itself, thus alleviating underlying neuroinflammation implicated as a central contributor to malaise, fatigue, brain fog, emotional reactivity, and other psychological symptoms. This revelation casts significant doubt on the broadly accepted model for the pathology of depression that classically purports serotonin deficiency as the primary cause. Today, a new breed of antidepressants specifically intended as anti-inflammatory drugs are undergoing feverish development by major drug corporations.
But before we herald these pharmaceutical innovations as the ultimate solution to tame the treachery of chronic neuroinflammatory disease, we must address the unjust marginalization and criminal victimization of disaffected Americans self-medicating via naturopathic means. Notwithstanding their evolutionary, anthropological, and social significance, the potent anti-inflammatory effects of cannabis, psilocybin mushrooms, and other psychedelic derivatives are now well-supported by an ever-growing body of recent scientific research. Although prohibitionist laws previously precluded a thorough investigation of their potential, the US has slowly and begrudgingly allowed the pursuit of psychedelic pharmacological power. As the barriers of outdated, impermissible, and fallacious legislative paradigms fall, clinicians are finally gaining critical insights that have enabled the development of novel pharmaceutical psychedelic derivatives with extreme precision; such that specific medical characteristics like an anti-inflammatory effect or psychedelic effect may be intentionally targeted and enhanced or diminished.

However new this scientific perspective may seem, medicinal preparations of psychedelics have reportedly been used for centuries, and even pharmaceuticals investigated and approved for clinical use decades ago were arguably directly modeled after psychedelics like LSD and psilocybin. Most notable of these compounds, Methergine (methylergometrine), is an LSD derivative used to induce contractions during childbirth since 1582, and is currently included on the World Health Organization’s (WHO) List of Essential Medicines. A similarly indispensable class of pharmaceutical psychedelic derivatives, the triptans, were first developed and patented in 1991 to treat migraines and cluster headaches, conditions which are both implicated to be caused by neuroinflammation. Interestingly, early triptans display remarkable structural similarities to tryptamine psychedelics like DMT and psilocybin.
Further progress spearheaded by brave and dutiful psychonauts in professional practice, underground social circles, and beyond has steadily illuminated the psychological and pharmacological nuances of many psychedelic drugs, revealing that they’re in fact highly safe and effective treatments for Post-Traumatic Stress Disorder (PTSD), suicidality, depression, anxiety, addiction, Fibromyalgia, various chronic inflammatory diseases, and more. Tireless efforts across decades of clinical trials using psychedelics such as cannabinoids, MDMA, ketamine, and psilocybin have paved the way to their current or imminent approval by the US Food and Drug Administration (FDA).
It finally seems quite possible that psychedelic medicines previously incorrectly admonished as “psychomimetic drugs” that imitated psychosis, damaged DNA, and were toxic to the human body may soon be available as legitimate pharmaceutical compounds aiming to alleviate the suffering of millions. With the current medical and legal trajectories, it’s highly likely that sometime in the not-so-distant future, inflamed Americans in need of psychedelic therapies will be able to access them without the unnecessarily harmful (but now still-looming) threat of social, criminal, and civil persecution. As much as one author celebrates this opportunity for a modicum of much needed progress in the United States, a single question remains:
Do a handful of state-level decriminalization initiatives for some select drugs, as well as the monetization and regulation of a limited number of pharmaceutical psychedelics at the federal level truly represent a sufficiently compassionate and broad solution to remedy the innumerable and egregious offenses against American life, liberty, and the pursuit of happiness committed by the war on drugs?
In this episode, Kyle interviews Dr. Jennifer Montjoy: Tucson, Arizona-based psychiatric nurse practitioner with a private practice specializing in ketamine-assisted psychotherapy, and Medical & Research Director at TRIPP (Transpersonal Research Institute of Psychotherapeutic Psychedelics); a 501(c)(3) organization that provides psychedelic training and research opportunities largely for female and BIPOC scientists.
A Vital student introduced Kyle to Montjoy’s research on ketamine and PTSD and presented with her at the recent ICPR conference in Amsterdam, where this was recorded in-person (as Kyle and Johanna were there, representing Psychedelics Today). Montjoy talks about her protocol, the self-transcendent scale she’s using with clients pre- and post- induction, how ketamine can help people get over past trauma through shifts in emotional memory, and what she sees most in successful cases: a gradual shift toward self-agency.
She discusses how integral titration is to her process; how ACE (adverse childhood experience) scores work; how dissociation can help with childhood trauma; how clients often naturally fall into using Internal Family Systems to describe their process; and how physicians and therapists shouldn’t be afraid of the concept of ceremony and opening sessions with intention – and, as she likes to say, giving one’s mind coordinates on where it can end up.
“I do think it’s helpful to have a skillset and general understanding of that so you know what’s happening in real time, but for the most part, I subscribe to the philosophy that we all have an inner healer. We all have that inner wisdom, but most of us don’t have access to it because we have these managing protectors from our trauma.”
“Often [for the] opening, I’ll ask the higher self to step into the light, to take the reins and let all those parts know that the goal here is not to annihilate or bypass them. That’s the language I consistently use in opening, because as the facilitator, we want to align with those parts too. We’re not the enemy.”
“Don’t be afraid to incorporate ‘ceremony.’ …I think that makes a lot of physicians maybe uncomfortable; that idea. [But] opening and closing [the ceremony] can be very helpful tools, [and] making sure we’re asking about intention before each session. I call that the coordinates, because we want to give the unconscious mind the coordinates.”
TrippAZ.org: The Transpersonal Research Institute of Psychotherapeutic Psychedelics
Resiliencetucson.com: 4-Day Experiential Training in Ketamine-Assisted Psychotherapy For Clinicians
Psychedelics Today: Ketamine and Trauma Treatment
Ncjfcj.org: Finding Your ACE Score
Psychedelics Today: PT300 – Dr. Richard C. Schwartz – Vital Psychedelic Conversations
Psychedelics Today: Veronika Gold – Methods of Ketamine Assisted Psychotherapy

In this episode, Joe interviews Christopher Dawson & Andrew Galloway: Co-Founders and CEO and COO, respectively, of Dimensions; a Canadian-based company creating retreats that blend traditional plant ceremonies with neuroscience and a luxurious, five-star environment.
Dawson realized what so many people were starting to learn about psychedelics after attending a 2015 conference in Peru that mixed neuroscientists with traditional healers, but for Galloway, it was direct experience, as he gives credit to plant medicines for helping him to heal from a 6-year addiction to crack cocaine. They each tell their story and how it led to the beginnings of Dimensions, where they worked for a year with a “Dreamlab” team of MDs, psychiatrists, practitioners from different fields, and even a design agency to create different programs for different substances – all with a focus on true set and setting and integrating perfectly with nature. They’re in the middle of a soft launch right now, offering cannabis in a ceremonial, group setting context to friends and families at their Algonquin Highlands location; perfecting everything before opening up to the general public. And once the law catches up with them, they hope to offer psilocybin and other psychedelic-assisted therapy across several new retreat locations.
They talk about Health Canada and the country’s trajectory towards legal psychedelics; critiques of traditional addiction treatment and the efficacy of 12-step programs; the tension between the psychedelic space and traditional healing space; investing in biotech; the polyvagal theory; how animals deal with trauma (and how we don’t); and the concept of integration: If you’re just taking a pill and not doing the work, are you missing the point entirely?
“We’re biased (we’re in the retreat business), but I don’t think that psilocybin, as an example, should be reduced to a pill that you take with your juice in the morning and you no longer take your SSRI because this is your new pill. For us, it’s the psychedelic-assisted therapy that actually maximizes the potential of the psychedelic experience, and that’s the mechanisms through which fundamental, behavioral change can take place. I think the idea that a pill can replace all of that means that you’re kind of missing the point about the whole experience.” -Chris
“I don’t want to slam traditional treatment because it actually did work for me to some degree. …I had a crack-cocaine addiction for six-seven years and ended up in rehab for six months and came back and participated in 12-step programs and remained abstinent. That part worked. The difference for me when I got involved with plant medicine was something else: I got healed. Instead of just abstaining and not using to cope or to manage with whatever I was dealing with, I actually healed through plant medicine.” -Andrew
“Is it a pill or is it the therapeutic process? If you don’t engage in integration, then you’re just taking a pill.” -Chris
“We talked about stigma earlier; it’s changing, and [for] the general public, the stigma around the war on drugs is changing too. I think people have finally figured out that it doesn’t work. No war works. We only declare war on things that we can make money from.” -Andrew
Dimensionsretreats.com: Algonquin Highlands
Psychedelics Today: PT314 – Daniel McQueen, MA – Vital Psychedelic Conversations
Psychedelics Today: Canada’s SAP Expansion Signals a Step Forward for Psychedelics
Dimensionsretreats.com: Dimensions + Queen’s University
Somaticmovementcenter.com: What is the Polyvagal Theory?
Psychedelics Today: PT248 – Pierre Bouchard – Somatic Therapy, Trauma, and the Nervous System (more about the polyvagal theory)
Psychedelicmedicinecoalition.org
 Christopher Dawson is the Co-Founder and CEO of Dimensions, a growing collection of retreat destinations combining neuroscientific research with plant ceremony in immersive natural environments. Prior to co-founding Dimensions, Christopher was the founder and CEO of Edgewood Health Network, where he oversaw the largest private network of residential/outpatient treatment providers in Canada and led the merger and acquisition of Canada’s top three treatment centers to create that network.
Christopher Dawson is the Co-Founder and CEO of Dimensions, a growing collection of retreat destinations combining neuroscientific research with plant ceremony in immersive natural environments. Prior to co-founding Dimensions, Christopher was the founder and CEO of Edgewood Health Network, where he oversaw the largest private network of residential/outpatient treatment providers in Canada and led the merger and acquisition of Canada’s top three treatment centers to create that network.
 Andrew Galloway is the Co-Founder and COO of Dimensions, a new paradigm for healing, combining ancient ceremonial plant medicines with modern science in safe, legal, and nurturing natural environments. He leads the organization’s clinical teams and operations for Dimensions Retreats, a new collection of immersive, transformational healing retreats combining neuroscientific research with plant ceremony and luxurious hospitality. Prior to co-founding Dimensions, he was a National Director of Edgewood Health Network; leading 10 outpatient centers. Andrew was the former VP at GreeneStone Muskoka, an international certified alcohol and drug counsellor, and has 14 years of experience working directly for the NHL/NHLPA substance abuse program.
Andrew Galloway is the Co-Founder and COO of Dimensions, a new paradigm for healing, combining ancient ceremonial plant medicines with modern science in safe, legal, and nurturing natural environments. He leads the organization’s clinical teams and operations for Dimensions Retreats, a new collection of immersive, transformational healing retreats combining neuroscientific research with plant ceremony and luxurious hospitality. Prior to co-founding Dimensions, he was a National Director of Edgewood Health Network; leading 10 outpatient centers. Andrew was the former VP at GreeneStone Muskoka, an international certified alcohol and drug counsellor, and has 14 years of experience working directly for the NHL/NHLPA substance abuse program.



In this episode, recorded in-person at the recent From Research to Reality summit, David interviews one of the more well-known figures in the psychedelic space (who somehow hasn’t been on the show yet), David Nutt: Psychiatrist, Founder and Chief Scientific Officer at Drug Science, Chief Research Officer at Awakn Life Sciences, and Edmund J. Safra Professor of Neuropsychopharmacology in the Division of Brain Science, Dept of Medicine, Imperial College London.
At Awakn Life Sciences, amongst other projects, Nutt is working to set up clinics for legal psychedelic therapy (so just ketamine for now), and, after a successful study on MDMA in the treatment of alcohol use disorder, he’s doing something nobody has really done before in seeing if improvements can be made to MDMA. He tells the story of when he was fired as chair of the Advisory Council on the Misuse of Drugs due to telling the truth about the differences in harm between alcohol, tobacco, and “bad” drugs like LSD and cocaine, which led to the birth of Drug Science (and embracing the truth about drugs even more).
He covers a lot of ground in this episode: how serotonin seems to affect the default mode network; glutamate, cortexes, and the flexibility in the human brain; Robin Carhart-Harris’ “Trial of Psilocybin versus Escitalopram for Depression” study and the realization that psychedelics were doing something different in the brain; Measure 109 and the importance of how Oregon establishes a new paradigm around legal mushrooms; drug hysteria in the US and UK and how drastically that differs from Portugal’s incredibly successful approach to drugs; why real world evidence is the core of science; and why psychedelics seem best at disrupting internalizing disorders.
“The reality is that the psychedelic impact on depression has been so powerful, it’s changed the whole narrative about how we think about depression. Our one study in [treatment]-resistant depression spawned 40 companies now [that] are working on psilocybin for depression, which is amazing. …It’s been a spark to this amazing expansion. Why? Because for the last 40 years, there’s not been any innovation in terms of mechanisms in treating depression, ever. All the drugs we have today are essentially safer derivatives of the drugs we invented in the 1950s. So this is a new approach, and that’s really, really exciting.”
“We’ve got to get our politicians, our policymakers to admit that these drugs should never, ever have been put in Schedule I. They were put in Schedule I [because] we said they were ‘very harmful’ (which they’re not), and they have no medical value (which they do), and it’s actually immoral now, reprehensible that politicians could not see that.”
“They just said, ‘Let’s try a different approach. Let’s try decriminalization and let’s treat drug addicts as human beings and help them get off the addiction rather than put them in prison.’ And that’s been one of the greatest success stories in the history of drug interventions. In the 15 years we have data since the Portuguese experiment was instigated, the Portuguese have reduced opiate deaths to one third of what they were before. In the same 15 years in Britain, using prohibitionist policies, we’ve doubled our deaths from opiates. And that, frankly, is an insult to humanity that we’ve pursued policies which we know are actually killing people.”
“Real world evidence is the core of medicine.”
New England Journal of Medicine: Trial of Psilocybin versus Escitalopram for Depression
Pubmed: Psilocybin for treatment-resistant depression: fMRI-measured brain mechanisms
Parea.science: Psychedelics Access and Research European Alliance
Nature.com: Sacked science adviser speaks out
BBC.com: Alcohol ‘more harmful than heroin’ says Prof David Nutt (with drug harm scale)
EJI.org: Nixon Adviser Admits War on Drugs Was Designed to Criminalize Black People
NPR.org: New York City allows the nation’s 1st supervised consumption sites for illegal drugs
NYTimes.com: How a Man With a Van Is Challenging U.K. Drug Policy
The Drug Science Podcast: #32 – Drug Consumption Rooms, with Peter Krykant
 David Nutt is a psychiatrist and the Edmund J. Safra Professor of Neuropsychopharmacology in the Division of Brain Science, Dept of Medicine, Imperial College London. There, he uses a range of brain imaging techniques to explore the causes of addiction and other psychiatric disorders and to search for new treatments. He has published over 400 original research papers, a similar number of reviews and books chapters, eight government reports on drugs, and 36 books, including one for the general public, Drugs: Without The Hot Air, that won the Transmission Prize in 2014.
David Nutt is a psychiatrist and the Edmund J. Safra Professor of Neuropsychopharmacology in the Division of Brain Science, Dept of Medicine, Imperial College London. There, he uses a range of brain imaging techniques to explore the causes of addiction and other psychiatric disorders and to search for new treatments. He has published over 400 original research papers, a similar number of reviews and books chapters, eight government reports on drugs, and 36 books, including one for the general public, Drugs: Without The Hot Air, that won the Transmission Prize in 2014.
He is currently the President of the European Brain Council and Founding Chair of Drug Science. Previously he has been president of the British Association of Psychopharmacology, the British Neuroscience Association, and the European College of Neuropsychopharmacology. He broadcasts widely to the general public both on radio and television. In 2010, The Times Eureka science magazine voted him one of the 100 most important figures in British Science, and the only psychiatrist in the list. In 2013, he was awarded the John Maddox Prize from Nature/Sense about Science for standing up for science.
Socials:
Twitter: David Nutt / Drug Science / Awakn Life Sciences



In this episode of the podcast, Joe interviews the CEO of Mindset Pharma, James Lanthier.
Mindset Pharma is a 3-year old biotechnology company built on discovering and developing new psychedelic compounds to be used as medicine for a variety of indications. While the efficacy of the psychedelics we know can’t be denied, the goal of science is to improve, and Lanthier believes optimizing these drugs will make them safer, more predictable, and more palatable for a far greater portion of the population. He envisions these new molecules leading to a future of highly personalized medicine, where people who would never eat a mushroom would likely take a related drug prescribed by their doctor.
Lanthier discusses what’s going on at Mindset Pharma; why patents alone will not be sufficient protection from competition; the long game of biotech, psychedelic stocks, and overreaction to slow growth; the Nagoya protocol; mescaline; the need for big pharma and capitalism; the art of formulation; and how microdosing could soon be revolutionized.
“I had some fairly well-known psychedelic investors say to me, ‘You’re just building a better mousetrap.’ And my reaction was: ‘Well, that’s the march of science. That’s what science is trying to do.’ Take the example of what the German scientist [Felix Hoffman] did in the nineteenth century to go from the bark of the willow tree, eventually going through a whole bunch of intermediate chemical steps to eventually get to Aspirin. Science hopefully tries to make things better, and that’s what we’re trying to do.”
“Big pharma has skipped right past psilocybin. Why? In my view, it would be because of the lack of strong IP rights. They’ve gone right to second and third generation drugs because they’ve made the assessment that even if you own the strongest IP in the psilocybin space, you’re still quite exposed, ultimately, to competition.”
“I think if there’s a future where you have relatively low-priced classic drugs potentially available alongside more optimized, specific drugs that have the full support of the medical community, that would be a great place to get to, I think – really great place to get to. And I think we only really get there with the machinery of capitalism moving forward.”
Otsuka-us.com (Otsuka Pharmaceutical)
Sciencehistory.org: Felix Hoffman
Protests for Right to Try (sent to us by Kathryn Tucker)
 James Lanthier is the CEO of Mindset Pharma, and is a seasoned technology executive with strong expertise in corporate finance, public markets and M&A. Most recently, Mr. Lanthier was a co-founder and CEO of Future Fertility, an innovative early stage developer of AI applications for human infertility. As a C-Suite executive, Mr. Lanthier has assisted in the growth and successful exit of numerous technology-enabled businesses through the public markets, including Mood Media, the world’s largest in-store media provider, and Fun Technologies, a pioneer in online casual games.
James Lanthier is the CEO of Mindset Pharma, and is a seasoned technology executive with strong expertise in corporate finance, public markets and M&A. Most recently, Mr. Lanthier was a co-founder and CEO of Future Fertility, an innovative early stage developer of AI applications for human infertility. As a C-Suite executive, Mr. Lanthier has assisted in the growth and successful exit of numerous technology-enabled businesses through the public markets, including Mood Media, the world’s largest in-store media provider, and Fun Technologies, a pioneer in online casual games.
Socials: Linkedin



In this episode, Joe interviews Julie Zukof: Head of Strategic Partnerships for Nue Life and the creator of Psychedelic Women, and Michelle Weiner: a double board-certified Doctor specializing in integrative pain management, using cannabis, ketamine, and other holistic modalities to get to the root cause of chronic pain.
Weiner tells of how her pain-management methods changed as her patients told her about the healing power of cannabis and ketamine, and how she was even more inspired by learning how much chronic pain is a result of fight-or-flight trauma reactions and resulting learned behavior. She discusses the central sensitization of fibromyalgia; ketamine infusions and dose discovery; the differences between how therapists and coaches are viewed (and the need for both); session music and trusting the facilitator in their music choice; and the importance of preparing for a ketamine experience through meditation and/or breathwork.
And they talk about Psychedelic Women, which was just founded in January as a result of Zukof realizing how much women were a minority in the psychedelic space. She talks about why we need more women in psychedelia; women’s natural inclination to connect and support each other; and how medicine should mirror that – where people from all methodologies can work together for the betterment of the patient. Psychedelic Women is in the process of updating from a speaker series to a more community-based platform. If you want to become a part of the community, sign up at their waitlist today!
“Personally, the coaches and the therapists that I use (my nurse practitioners) are mainly women. And I don’t know if that’s because they gravitate towards this field or because patients gravitate towards them, but there’s that nurturing, innate property of being a woman that also is special and unique and we can use to our advantage in that sense.” -Michelle
“I think people are under the impression that psychedelics are always meant to be enjoyable. And while ketamine oftentimes is enjoyable, sometimes it’s meant to be part of a healing journey.” -Julie
“I credit Dustin [Robinson] for bringing us on and featuring the group at Soho House, and something he said was, ‘It’s not that I don’t want to feature women on the panel, I just need more women in the space to feature them.’ And I think that’s an excellent point. And if we can help do something about that, then I think we’re winning.” -Julie
“There’s so many other people that are involved in making this experience more effective for people. It’s not just the medicine and the doctor and the therapist and the coach. …It’s so nice to see because this is really how medicine should be. It shouldn’t be everybody in their own box like with other physicians. …This whole group is really bringing people together that have certain talents and passions and saying: ‘We can work together.’” -Michelle
Psychedelics Today: PTSF 41 (with Mendel Kaelen of Wavepaths)
“Psychedelics & Pain Symposium” event by REMAP Therapeutics (this event is tomorrow!)
Stanford Psychedelic Science Group
UC San Diego: Psychedelics and Health Research Initiative
 Julie Zukof is the creator of Psychedelic Women, a speaker series and influential community. Over her eighteen year career in NYC, Julie has created, innovated, marketed, and grown wellness brands by working at prestigious innovation firms and then starting her own consultancy. Julie is now Head of Strategic Partnerships for Nue Life, the leading mental wellness company in at-home ketamine treatments.
Julie Zukof is the creator of Psychedelic Women, a speaker series and influential community. Over her eighteen year career in NYC, Julie has created, innovated, marketed, and grown wellness brands by working at prestigious innovation firms and then starting her own consultancy. Julie is now Head of Strategic Partnerships for Nue Life, the leading mental wellness company in at-home ketamine treatments.
Socials:
 Dr. Michelle Weiner is double board-certified in Interventional Pain Medicine and Physical Medicine and Rehabilitation, and a partner in private practice at Spine and Wellness Centers of America. She is a member of Florida’s Medical Cannabis Advisory Committee, vice president of Mr. Psychedelic Law, a not-for-profit with the mission of responsible legal reform of psilocybin, and a clinical advisor for Iter Investments, a venture capital firm focused on supporting emerging companies within the psychedelic ecosystem of behavioral and mental health. Dr. Weiner’s research focuses on using cannabis as a substitute for opioids in chronic pain patients and cannabis’s effect on seniors with chronic pain, as well as comparing psychedelic v psycholytic doses of ketamine for chronic pain and depression. Her unique approach of personalized and preventative medicine focuses on empowering her patients to cultivate health using cannabis and ketamine-assisted psychotherapy as a catalyst to identify the root cause of one’s suffering, optimizing their quality of life.
Dr. Michelle Weiner is double board-certified in Interventional Pain Medicine and Physical Medicine and Rehabilitation, and a partner in private practice at Spine and Wellness Centers of America. She is a member of Florida’s Medical Cannabis Advisory Committee, vice president of Mr. Psychedelic Law, a not-for-profit with the mission of responsible legal reform of psilocybin, and a clinical advisor for Iter Investments, a venture capital firm focused on supporting emerging companies within the psychedelic ecosystem of behavioral and mental health. Dr. Weiner’s research focuses on using cannabis as a substitute for opioids in chronic pain patients and cannabis’s effect on seniors with chronic pain, as well as comparing psychedelic v psycholytic doses of ketamine for chronic pain and depression. Her unique approach of personalized and preventative medicine focuses on empowering her patients to cultivate health using cannabis and ketamine-assisted psychotherapy as a catalyst to identify the root cause of one’s suffering, optimizing their quality of life.
Socials: Instagram



In this episode, Joe interviews Co-Founder and CEO of Sensorium Therapeutics, Dick Simon.
Sensorium Therapeutics was created by professionals from Massachusetts General Hospital who started to wonder: With so many plants with rich, ethnobotanical history, what if we looked to those plants for answers instead of just analyzing the trendy psychedelics so many are focused on now? Why not fully research what already has established efficacy? Their goal is to have the largest collection of psychoactive plants (which they’re calling their Neuro-Natural Library), and use machine learning to figure out exactly which molecules are doing what, to then synthesize new drugs that are safe and effective; eventually bringing these new compounds through the FDA approval process.
Simon talks about how so much of what we know to be effective and beneficial is based on assumptions or best guesses, and while that doesn’t discredit very real benefits, it does beg the question: Is this all optimized as best as it could be?
He also discusses how recent advances in neuroscience and technology are catalyzing molecular research; how we can learn about other mental health indications from studying rumination; the benefits and challenges of nutraceuticals; geopolitical conflict resolution; organoids; the necessity of the FDA; why “them” can be a very dangerous word; the challenges of benzodiazepines; Burning Man; and the problem with people needing to be treatment-resistant or seriously ill to gain access to psychedelics. He hopes that what Sensorium Therapeutics learns over the coming years will help bring better medicines to more people.
“The goal here is to look at the 500+ plants and fungi and what their component elements are (what’s actually driving that efficacy, or signals of efficacy; signals that they make a difference in a high throughput way), to really assemble massive data. Then, we’re using machine learning to distill all that down to: ‘Alright, we have all this cool information; what does it mean? What does it tell us? And how do we convert that into a drug that helps people?’”
“We operate under a lot of assumptions that are based on experience, but are not based on any controls on the experience. Even something basic like the assumption [that] music and playlists are really important – they’ve been used and they seem to work. We don’t really know if that’s true. …I’m not saying that music and a controlled playlist isn’t absolutely the best answer, but it seems like it’s something we really ought to know an answer to, rather than make assumptions.”
“If I would have told someone ten years ago: “No, no, we’re going to have this company, Sensorium, and it is going to be able to, in a 384-well plate, take a look at groups of neurons growing, and we’ll have sophisticated microscopy to take a look at it, and we’ll be able to do it at a high throughput basis, and we can reliably do it and replicate,’ the question would have been: ‘Alright, what other drugs are you taking? That’s not going to [happen].’ [But] we’re there.”
“Even questions as to how important the psychedelic effect is to efficacy; the assumption tends to be that somehow or another, the intensity of the experience is related to the efficacy. …There are people now who are looking at: ‘What if you removed the psychedelic effect from psychedelics? Are you still getting the same neuroplasticity, neurogenesis, and much of the effect?’ I don’t know the answer, but I think those that are ideologues on either side of that [are] silly. Let’s figure it out. …Why don’t we find the answer rather than argue for whatever our position is?”
Massachusetts General Hospital Center for the Neuroscience of Psychedelics
Psychedelics Today: PT245 – Robin Carhart-Harris – Psychedelics, Entropy, and Plasticity
The Nagoya Protocol on Access and Benefit-Sharing
Dick Simon Ted Talk: ”The Most Dangerous Four Letter Word: Them”
An Intellectual History of Psychology, by Daniel N. Robinson
Bostonpsychedelicresearchgroup.com
 Dick Simon is a serial entrepreneur and leader in advancing psychedelic-assisted therapies. He is the Chairman of the Advisory Council of Center for the Neuroscience of Psychedelics at Massachusetts General Hospital, Co- Founder and Board Member of the Boston Psychedelic Research Group, and on the steering committee for the Psychedelic Science Funders Collaborative. He received his undergraduate degree from Cornell University and his MBA from Harvard Business School. After September 11, 2001, he co-founded and led the YPO Peace Action Network which leverages personal and business relationships, resources, and expertise for conflict resolution on local and global levels. Dick’s work has earned him YPO’s Global Humanitarian Award, Harvard Business School’s Making a Difference Award, inclusion in Real Leaders magazine’s “100 Visionary Leaders” and in the “100 Most Influential People in Psychedelics” list.
Dick Simon is a serial entrepreneur and leader in advancing psychedelic-assisted therapies. He is the Chairman of the Advisory Council of Center for the Neuroscience of Psychedelics at Massachusetts General Hospital, Co- Founder and Board Member of the Boston Psychedelic Research Group, and on the steering committee for the Psychedelic Science Funders Collaborative. He received his undergraduate degree from Cornell University and his MBA from Harvard Business School. After September 11, 2001, he co-founded and led the YPO Peace Action Network which leverages personal and business relationships, resources, and expertise for conflict resolution on local and global levels. Dick’s work has earned him YPO’s Global Humanitarian Award, Harvard Business School’s Making a Difference Award, inclusion in Real Leaders magazine’s “100 Visionary Leaders” and in the “100 Most Influential People in Psychedelics” list.
Socials: Instagram / Twitter / Facebook / Linkedin



In this bonus episode, Kyle interviews Dr. Scott Shannon: psychiatrist, Founder of Wholeness Center in Fort Collins, CO, and Co-Founder and CEO of the Board of Psychedelic Medicine and Therapies (BPMT); a non-profit public benefit corporation which was recently created to certify healthcare professionals in psychedelic-assisted psychotherapy – and which was just in the news last week when they received a $900,000 matching grant from the Steven & Alexandra Cohen Foundation.
Shannon feels that the majority of people who are interested in (and could benefit from) psychedelics would prefer that their experience be as close to a conventional medical setting as possible. And especially with the risks of rogue practitioners, licensing boards want to see predictability, uniformity, regulation, and (perhaps most importantly) that we as a psychedelic culture are placing importance on being accountable and self-governing. He wants to establish a certification process that’s standard enough that which medicine the patient is using will become secondary.
He discusses what the certification process will likely look like; why uniformity is so important; the challenges of respecting and integrating Indigenous traditions into a medical model that’s drastically different; what people should look for in psychedelic education; and the importance of breaking from a siloed and hierarchical model into one that’s cross-disciplinary, where professionals of all types can work together for the betterment of the patient.
“The premise of the certification board is that we’re trying to certify a process …of medication-assisted, psychedelic-assisted psychotherapy that looks at integration [and] prep, that looks at set and setting, that looks at the sacred container of this relationship; and that we build that, and that is the core of it, and the medications become a little bit secondary. We can bring ketamine in, we can bring DMT in, we can bring psilocybin [in], [and] we can bring MDMA in; because these medications, frankly, they’re not really chemically-related or that similar, but what’s similar is the process that patients go through with them.”
“There’s always the question of: ‘How do I get training?’ …The Psychedelic Science Funders Collaborative just did a survey of the field of education and found that there are now over 50 providers of psychedelic education, and four years ago, there might have been a handful. But someone coming [up]: What do they do? ‘How much do I need to study?’ These things are expensive. It’s confusing. So we want to create a clear, professional path [where] someone says: ‘I’m going to step into this and do this as a career. Here’s what I need to do? Good. I can do that.’”
Psychedelicsboard.org (The Board of Psychedelic Medicine and Therapies (BPMT))
Wholeness.com (Wholeness Center)
Psychedelics Today: Dr. Scott Shannon – Ketamine Therapies
 Scott has been a student of consciousness since his honor’s thesis on that topic at the University of Arizona in the 1970s. Following medical school, MDMA-assisted psychotherapy became a facet of his practice before this medicine was scheduled in 1985. He then completed a Psychiatry residency at a Columbia program in New York. Scott studied cross-cultural psychiatry and completed a child/adolescent psychiatry fellowship at the University of New Mexico. Scott has published four books on holistic and integrative mental health including the first textbook for this field in 2001. He founded Wholeness Center in 2010 with a group of aligned professionals to create innovation in collaborative mental health care.
Scott has been a student of consciousness since his honor’s thesis on that topic at the University of Arizona in the 1970s. Following medical school, MDMA-assisted psychotherapy became a facet of his practice before this medicine was scheduled in 1985. He then completed a Psychiatry residency at a Columbia program in New York. Scott studied cross-cultural psychiatry and completed a child/adolescent psychiatry fellowship at the University of New Mexico. Scott has published four books on holistic and integrative mental health including the first textbook for this field in 2001. He founded Wholeness Center in 2010 with a group of aligned professionals to create innovation in collaborative mental health care.
Scott is a past President of the American Holistic Medical Association and a past President of the American Board of Integrative Holistic Medicine. He serves as a site Principal Investigator and therapist for the Phase III trial of MDMA assisted psychotherapy for PTSD sponsored by Multidisciplinary Association for Psychedelic Studies. He has also published numerous articles about his research on cannabidiol (CBD) in mental health. Scott founded the Psychedelic Research and Training Institute (PRATI) to train professionals in ketamine-assisted psychotherapy and deliver clinically relevant studies. Scott co-founded the Board of Psychedelic Medicine and Therapies in 2021 and currently serves as the CEO for this non-profit public benefit corporation. He lectures all over the world to professional groups interested in a deeper look at mental health issues and a paradigm shifting perspective about transformative care.



In this episode, David interviews one of the biggest names in psychedelics and someone we haven’t had on the show until now; Founder and Executive Director of the Multidisciplinary Association for Psychedelic Studies (MAPS), Rick Doblin, Ph.D.
MAPS has recently been at the center of media scrutiny, notably through the New York magazine‘s “Cover Story” podcast series, which chronicled instances of alleged sexual abuse within the MAPS clinical MDMA trials. Since reporting on this issue has largely called into question the design of MAPS’ clinical trials, data reporting, quality control, and claims around the efficacy of MDMA in the treatment of PTSD, we wanted to provide an opportunity for Doblin to respond to these very real concerns – and he does just that.
He discusses how MAPS reacted, what could have been done better, what it has all meant for the non-profit, and how it feels to now be considered the enemy by many in a space MAPS helped build. He addresses the concerns of sessions ending too soon (highlighting how that may suggest a desire for additional therapy) and asks anyone who has participated in a MAPS trial to complete a long-term follow-up survey so the organization can improve their process and ensure their data is as accurate and robust as possible.
He also discusses what the post-approval psychedelic landscape could look like; their goals for facilitator training and how they align with requirements in Oregon; their desire for a patient registry or “global trauma index”; and the importance of collecting and analyzing real-world evidence. And he talks about MAPS and their globalization goals: how exploring psychedelic therapy specifically in countries with little to no tradition of psychotherapy can lead to new therapeutic models. Rather than exploring areas where there is guaranteed revenue, they are seeking areas that are high in trauma instead – to bring these medicines where they are most needed.
“I think you can have solutions that go too far. The podcast people put out a solution, saying that there should be no touch in therapy. …They’ve also said that [our] studies should be shut down and that we need experts to think about this for years. I think that kind of thinking is out of balance with the amount of suffering that seems to actually be alleviated.”
“The more dangerous the drug, the more important it is that it be legal.”
“We’re really wanting to bring this to the police, [and] we’ve done a lot of work with veterans. The breakthrough that we’re still looking forward to one day would be to treat the first active duty soldier. So far, it’s only been veterans, but if we can treat active duty soldiers, I think that would be [great]. The closer you can treat people to the trauma, probably the better.”
“Even though we’re focused on MDMA and there’s all these other things for MDMA, really, what we’re doing is opening the door to psychedelic medicine. So what we want, ideally, is therapists to be cross-trained with MDMA, ketamine, psilocybin, ibogaine, 5-MeO-DMT, ayahuasca, whatever. And then the psychedelic clinics of the future will not be: ‘Here’s a ketamine clinic, here’s [an] MDMA clinic, here’s a psilocybin clinic.’ It will be psychedelic clinics, and the therapists will be cross-trained and they’ll customize a treatment program for each individual patient with any number of different kinds of psychedelics at different times in a sequence.”
Thecut.com: You Won’t Feel High After Watching This Video
New York Magazine: Cover Story, Season One: Power Trip
Maps.org: Statement: Public Announcement of Ethical Violation by Former MAPS-Sponsored Investigators
Psychedelics Today: Addressing Abuse in Psychedelic Spaces
Fromresearchtoreality.com: Global Summit on Psychedelic-Assisted Therapies and Medicine
Psychedelics Today: Peter Hendricks Ph.D. – Is Psilocybin Helpful For People Who Abuse Cocaine?
Psychedelics Today: PT227 – Dr. Anne Wagner – Couples Therapy, MDMA, and MAPS
Psychedelicscience.org: June 17-25, 2023 in Denver
Psychedelics Today: PT236 – Dr. Carl Hart – Drugs: Honesty, Responsibility, and Logic
Forastateofhappiness.com: How is Gross National Happiness measured in Bhutan?
 Rick Doblin, Ph.D., is the founder and executive director of the Multidisciplinary Association for Psychedelic Studies (MAPS). He received his doctorate in Public Policy from Harvard’s Kennedy School of Government, where he wrote his dissertation on the regulation of the medical uses of psychedelics and marijuana and his Master’s thesis on a survey of oncologists about smoked marijuana vs. the oral THC pill in nausea control for cancer patients. His undergraduate thesis at New College of Florida was a 25-year follow-up to the classic Good Friday Experiment, which evaluated the potential of psychedelic drugs to catalyze religious experiences. He also conducted a 34-year follow-up study to Timothy Leary’s Concord Prison Experiment. Rick studied with Dr. Stanislav Grof and was among the first to be certified as a Holotropic Breathwork practitioner. His professional goal is to help develop legal contexts for the beneficial uses of psychedelics and marijuana, primarily as prescription medicines but also for personal growth for otherwise healthy people, and eventually to become a legally licensed psychedelic therapist. He founded MAPS in 1986, and currently resides in Boston with his wife, with three children who have all left the nest.
Rick Doblin, Ph.D., is the founder and executive director of the Multidisciplinary Association for Psychedelic Studies (MAPS). He received his doctorate in Public Policy from Harvard’s Kennedy School of Government, where he wrote his dissertation on the regulation of the medical uses of psychedelics and marijuana and his Master’s thesis on a survey of oncologists about smoked marijuana vs. the oral THC pill in nausea control for cancer patients. His undergraduate thesis at New College of Florida was a 25-year follow-up to the classic Good Friday Experiment, which evaluated the potential of psychedelic drugs to catalyze religious experiences. He also conducted a 34-year follow-up study to Timothy Leary’s Concord Prison Experiment. Rick studied with Dr. Stanislav Grof and was among the first to be certified as a Holotropic Breathwork practitioner. His professional goal is to help develop legal contexts for the beneficial uses of psychedelics and marijuana, primarily as prescription medicines but also for personal growth for otherwise healthy people, and eventually to become a legally licensed psychedelic therapist. He founded MAPS in 1986, and currently resides in Boston with his wife, with three children who have all left the nest.
Socials: Twitter / Instagram
MAPS socials: Twitter / Instagram



In this episode, David interviews Clinical Psychologist and Founder of the Psychedelic Society of Vermont, Dr. Rick Barnett, PsyD.
Barnett discusses the importance of building community in psychedelic spaces; psychedelic experiences as preventative medicine, and the differences between (and value within) the sanitized medical model and more ritualistic experiences. He talks about his own personal journey with addiction and recovery and looks at the interrelation between trauma, addiction, trust, and how psychedelics operate as disruptors – with a sense of meaning and purpose.
He discusses many of the current clinical trials happening around psychedelics and addiction; Alcoholics Anonymous and LSD; Vermont’s developing decriminalization bill (Measure H.644); the psychiatric workforce shortage and the potential solution of more prescribing psychologists; and, considering Oregon’s budding psilocybin therapy model, points out that one doesn’t need to be a licensed clinical practitioner with specific schooling to be a good psychedelic facilitator. Could we instead build models that are based largely on competency?
The Psychedelic Society of Vermont is putting on the Psychedelic Science & Spirituality Summit on the summer solstice (June 20-21) in Stowe, VT, with the goal of holding space for both the scientific and spiritual side of psychedelia. The conference is specifically for healthcare professionals, but all others are welcome to virtually attend or come to the summer solstice celebration after the conference. For more info, head to vermontpsychedelic.org.
“I had several profound experiences with LSD when I was a kid, and when I crashed and burned on alcohol and wound up in a 12-step rehab (the Hazelden Foundation), I quickly recognized that my experiences with LSD made me extremely receptive to the message that was being put forth to me in a 12-step-oriented rehab program. Concepts like surrender and a connection to spirituality, a connection to open-mindedness, willingness, being honest with oneself, taking one’s inventory – these kinds of concepts that are so common in 12-step programs – they resonated so strongly with me because of my experiences with LSD.”
“We have the ability to instill a sense of trust with our patients, and they can begin to trust themselves, and to trust the therapist, and to review some of these old hurts and really get into it over the course of therapy in a way that’s very healing. So it can happen with therapy, and I don’t think one is necessarily a substitute for the other. I think [psychedelics and therapy] work very well together. Psychedelics are yet another tool, just like therapy is a tool, just like AA is a tool, just like Suboxone and Methadone are tools. They’re all tools, and it’s really important to respect and honor that each one brings something positive, potentially, for an individual.”
“An AA program, a harm reduction program, a therapy program, a psychedelic program, [a] meditation retreat: All these things provide a nudge, and potentially a very transformative nudge in the direction of like, ‘Okay, and then what?’ What are you doing in your daily life? …That ‘assisted’ part is not just assisted by a therapist. It’s not just assisted by a drug. It’s not just assisted by a shaman or an integration coach. It’s assisted by everything.”
Psychedelic Science & Spirituality Summit
Openstates.org: An act relating to decriminalization of a personal use supply of a regulated drug
Psychedelics Today: PT236 – Dr. Carl Hart – Drugs: Honesty, Responsibility, and Logic
Hazelden.org: Hazelden Foundation
Mydecine.com: Mydecine Receives Conditional IRB Approval for Phase 2b Smoking Cessation Study
Pubmed: Long-term follow-up of psilocybin-facilitated smoking cessation
Lucid.news: Bill Wilson, LSD and the Secret Psychedelic History of Alcoholics Anonymous
His Linkedin post about trust and being let down
 Dr. Rick Barnett, Psy.D., is the Co-Founder of the Psychedelic Society of Vermont, the Legislative Chair and Past-President of the Vermont Psychological Association, the founder of the non-profit organization, CARTER, Inc., and is a clinical psychologist and addiction specialist in private practice in Stowe, VT. Dr. Barnett has worked as a Clinical Psychologist in nursing homes, hospitals, and outpatient programs, and has trained hundreds of health professionals through workshops on addiction and mental health issues over the past 20 years. He is in long-term recovery of alcohol and substance abuse and is an active advocate for addiction treatment and recovery resources. Dr. Barnett holds a Bachelor’s degree in psychology from Columbia University, a Doctorate and Master’s Degree in Clinical Psychology and a Master’s Degree in Clinical Psychopharmacology. He is a Licensed Alcohol and Drug Counselor and holds certificate in Problematic Sexual Behavior (PSB-S) and Gambling Disorder.
Dr. Rick Barnett, Psy.D., is the Co-Founder of the Psychedelic Society of Vermont, the Legislative Chair and Past-President of the Vermont Psychological Association, the founder of the non-profit organization, CARTER, Inc., and is a clinical psychologist and addiction specialist in private practice in Stowe, VT. Dr. Barnett has worked as a Clinical Psychologist in nursing homes, hospitals, and outpatient programs, and has trained hundreds of health professionals through workshops on addiction and mental health issues over the past 20 years. He is in long-term recovery of alcohol and substance abuse and is an active advocate for addiction treatment and recovery resources. Dr. Barnett holds a Bachelor’s degree in psychology from Columbia University, a Doctorate and Master’s Degree in Clinical Psychology and a Master’s Degree in Clinical Psychopharmacology. He is a Licensed Alcohol and Drug Counselor and holds certificate in Problematic Sexual Behavior (PSB-S) and Gambling Disorder.



In this episode of the podcast, Kyle interviews psychiatrist, Dr. Reid Robison, and clinical psychologist, Steve Thayer, Ph.D. Together, they host the Psychedelic Therapy Frontiers podcast and work at Novamind; Robinson as the Chief Medical Officer, and Thayer as the Clinical Director of Education & Training.
They talk about their respective journeys from psychology into the field of psychedelic medicine, their current work with ketamine-assisted psychotherapy (KAP) at Novamind, and their combined efforts in educating and training future KAP therapists and clinicians – a need they feel is going to become increasingly urgent as ketamine becomes more mainstream. To meet the challenge of scaling accessibility of psychedelic therapies, Novamind recently combined forces with Numinus Wellness, creating a platform and standard of mental health care within psychedelic therapy.
Robison and Thayer discuss the different ketamine dosing modalities and purpose for each; the ketamine sessions Novamind provides for frontline healthcare workers (called ‘Frontline KAP’ or FKAP); how difficulties in emotion-processing are often at the heart of mental health struggles; and how ketamine can help loosen emotional binding, allowing greater access to them. They also discuss current clinical trials on LSD for anxiety and alcoholism; how ketamine can be used for therapist burnout; the challenge of long LSD sessions and therapist stamina; the benefits of group ketamine sessions; the concept of combining ketamine with other therapeutic modalities (or substances); and the power of stepping aside and allowing the inner healer to take over.
“Difficulties in emotion processing are often at the heart of many mental health struggles. And if we can support the clients in developing skills and confidence in moving towards their emotions, and leverage the power of the corrective experience, the healing power of caregivers, [and] supporting them with emotion coaching skills, then we’re wrapping the client in this really powerful therapeutic healing environment and leveraging ketamine as a catalyst.” -Reid
“People will tend toward self-actualization and transcendence if you give them the environment to do so. To be well is not something we have to teach people to do, it’s something that they can remember how to do. It’s in them. If we can help them peel away the negative programming and conditioning and trauma and all that stuff, they’ll find their way to health and healing.” -Steve
“To me, it makes complete sense to use something like LSD for anxiety because what we think perpetuates something like generalized anxiety is what Steve Hayes of ACT might call ‘experiential avoidance’; that we don’t want to feel these intense feelings of fear or embarrassment or rejection or whatever it is, so we worry chronically, we get addicted to worry itself, [and that] keeps us safe from having to do scary stuff. And the LSD experience is just (for a lot of people) going to crack that open and give you an opportunity to face your fears, so to speak. It’s like exposure therapy on psychedelic steroids.” -Steve
Psychedelic Therapy Frontiers podcast
Foundations of KAP Training Course from Cedar Psychiatry
MAPS MDMA Therapy Training Program
Novamind.ca: Frontline KAP Group Sessions for Health Care Workers
Wholeness.com: Dr. Scott Shannon
Psychedelics Today: PT302 – Dr. Adele Lafrance – Vital Psychedelic Conversations
Psychedelics Today: PT300 – Dr. Richard C. Schwartz – Vital Psychedelic Conversations
 Dr. Reid Robison is a board-certified psychiatrist and Chief Medical Officer at Novamind. He is adjunct faculty at the University of Utah, founder of the Polizzi Free Clinic, co-founder of Cedar Psychiatry, the medical director for the Center for Change, and was voted Best Psychiatrist in Utah in 2020. Over the past decade, Dr. Robison has led over 200 clinical trials in neuropsychiatry. Notably, he served as Coordinating Investigator for the Multidisciplinary Association for Psychedelic Studies (MAPS) MDMA-assisted psychotherapy study of eating disorders. As an early adopter and researcher of ketamine in psychiatry, Dr. Robison led a pivotal IV ketamine study for treatment-resistant depression by Janssen, leading to FDA approval of Spravato™. Dr. Robison is also the co-host of the Psychedelic Therapy Frontiers podcast.
Dr. Reid Robison is a board-certified psychiatrist and Chief Medical Officer at Novamind. He is adjunct faculty at the University of Utah, founder of the Polizzi Free Clinic, co-founder of Cedar Psychiatry, the medical director for the Center for Change, and was voted Best Psychiatrist in Utah in 2020. Over the past decade, Dr. Robison has led over 200 clinical trials in neuropsychiatry. Notably, he served as Coordinating Investigator for the Multidisciplinary Association for Psychedelic Studies (MAPS) MDMA-assisted psychotherapy study of eating disorders. As an early adopter and researcher of ketamine in psychiatry, Dr. Robison led a pivotal IV ketamine study for treatment-resistant depression by Janssen, leading to FDA approval of Spravato™. Dr. Robison is also the co-host of the Psychedelic Therapy Frontiers podcast.
 Dr. Steve Thayer is a clinical psychologist and Clinical Director of Education & Training at Novamind. As a USAF military veteran, Dr. Thayer maintains his commitment to serving the veteran and first responder community through his position as the Executive Director of Therapeutic Operations for the World Voice Project. At Novamind, Dr. Thayer conducts and provides training in ketamine-assisted psychotherapy. He serves as Lead Therapist on several clinical trial studies involving psychedelic medicine. Dr. Thayer is also the co-host of the Psychedelic Therapy Frontiers podcast.
Dr. Steve Thayer is a clinical psychologist and Clinical Director of Education & Training at Novamind. As a USAF military veteran, Dr. Thayer maintains his commitment to serving the veteran and first responder community through his position as the Executive Director of Therapeutic Operations for the World Voice Project. At Novamind, Dr. Thayer conducts and provides training in ketamine-assisted psychotherapy. He serves as Lead Therapist on several clinical trial studies involving psychedelic medicine. Dr. Thayer is also the co-host of the Psychedelic Therapy Frontiers podcast.



In this episode of the podcast, Joe interviews retired Nurse Practitioner, Midwife, and Air Force Captain, Kimberly Juroviesky.
Juroviesky was forced to retire from her career and aspirations in the Air Force after she fell during a training exercise and again on ice months later, eventually realizing she had developed Complex Regional Pain Syndrome; a little understood condition where essentially, nerves continue to tell one’s brain that a healed injury should still hurt. When she tried ketamine and it cut her pain in half, she wondered, “Why aren’t more people doing this?” and created the Ketamine Task Force to fight to get insurance to pay for ketamine (and eventually, other legalized psychedelics).
She discusses Complex Regional Pain Syndrome and her path to ketamine; the redefining of “treatment-resistant”; the lack of knowledge from so many physicians about drug interactions and proper dosing; the mental health benefits of primal activities like swimming or dancing; the utility, timing, and efficacy of each ketamine method (for others and what’s worked best for her); the arduous and frustrating process of applying for a new CPT code with the AMA; how chronic pain and suicidality are intertwined; and the relationship between the timing of ketamine sessions, improvements, and problems returning.
Juroviesky is currently practicing Nue Life‘s protocol, with at-home ketamine and participating in group integration sessions. She believes the future of ketamine will be similar to how many feel psychedelics like ayahuasca, psilocybin, or LSD should be used: using smaller (and lighter) doses as maintenance in between larger experiences (in this case, in-office IV or ketamine infusions) – with, of course, lots of integration.
“The biggest hurdle has been access for me [and] access for everyone, because unfortunately, the majority of insurances refuse to pay for ketamine. It’s very depressing, very upsetting that you have all these people who could benefit but they can’t get access because they can’t afford it, because most of the people who need this medicine, unfortunately, are on disability and no one has the money to pay thousands upon thousands of dollars for this treatment. So I founded an organization called the Ketamine Task Force in order to fight to get insurances to cover ketamine.”
“Unfortunately, there’s so many clinicians out there who are either not telling their patients things like which drugs prevent ketamine from working at its best, or they’re doing doses that are so ridiculously low that their patients get no response and then their patients think they’ve ‘failed ketamine.’ And I’m like, ‘You haven’t even tried ketamine! You think you’ve failed it, but really, you’ve only gotten .2 milligrams per kilogram. That’s like taking a baby aspirin for a brain tumor.’ Education is so important; not just education for patients, [but] education for clinicians.”
“There are people who go into their ketamine treatment completely suicidal, with a plan, ready to kill themselves, and they come out and they say, ‘I don’t want to kill myself anymore.’ It’s unbelievable, the changes. Even in one session, it can reduce that suicidality. It doesn’t [work right away] for everyone. Sometimes it takes three, four, six, ten [sessions], but almost everyone sees some improvement immediately, and that’s the amazing thing. …And if it’s not ketamine, then, like I said: try psilocybin, try MDMA. But there is hope. Don’t give up hope. There’s always hope. As long as you’re alive, there’s always hope for tomorrow.”
“We want to be the go-to who’s going to help with ground-breaking and changing laws and getting things done. …We want to be the ones to bring it to the world because we just feel like this is so important. We literally are changing the world right now.”
Ketamine Task Force Facebook group
Medical Billing CPT Codes: What is CPT?
Imdb.com: Who Killed the Electric Car?
Psychedelics Today: Court Wing – Pain and Its Relationship to the Mind
Rollingstone.com: Naomi Judd Died by Suicide, Ashley Judd Reveals
 Kimberly Juroviesky is a retired Nurse Practitioner and Nurse Midwife who trained at Columbia University and The University of Medicine and Dentistry of New Jersey. She was injured on active duty while in the USAF and developed Complex Regional Pain Syndrome which unfortunately, forced her to retire from her career early. Kimberly began getting ketamine infusions in 2015 as part of a research study. While they don’t make her pain levels disappear, they do bring them down to what she describes as “livable levels.” Kimberly has always been driven to help people so she started up a Facebook group to support patients in their ketamine journeys. Kimberly also started a second Facebook group to allow ketamine providers to connect with one another. Kimberly also wrote a book to help patients to know what to expect during their infusions called Ketamine Infusions: A Patient’s Guide. She also is the author of Ketamine Journeys: A Journal for Your Ketamine Experiences. Kimberly has found a new passion in being an advocate for the use of ketamine to treat both mental health and pain diagnoses. She advocates for and talks with both patients and providers around the globe on a daily basis.
Kimberly Juroviesky is a retired Nurse Practitioner and Nurse Midwife who trained at Columbia University and The University of Medicine and Dentistry of New Jersey. She was injured on active duty while in the USAF and developed Complex Regional Pain Syndrome which unfortunately, forced her to retire from her career early. Kimberly began getting ketamine infusions in 2015 as part of a research study. While they don’t make her pain levels disappear, they do bring them down to what she describes as “livable levels.” Kimberly has always been driven to help people so she started up a Facebook group to support patients in their ketamine journeys. Kimberly also started a second Facebook group to allow ketamine providers to connect with one another. Kimberly also wrote a book to help patients to know what to expect during their infusions called Ketamine Infusions: A Patient’s Guide. She also is the author of Ketamine Journeys: A Journal for Your Ketamine Experiences. Kimberly has found a new passion in being an advocate for the use of ketamine to treat both mental health and pain diagnoses. She advocates for and talks with both patients and providers around the globe on a daily basis.
Socials: Twitter / Linkedin / Instagram



In this episode of the podcast, Joe interviews Lyle Maxson: Co-Founder and Chief Strategy Officer of Entheo Digital, a “technodelic” company focusing on digital therapeutics and virtual reality – both as adjuncts to psychedelic-assisted therapy, and theoretically, as new forms of medicine.
Maxson began his career by creating immersive, psychedelic-like experiences at some of the world’s largest music festivals. It was mostly those world-building experiences and some time in sensory deprivation tanks that led to his interest in seeing just what was possible through altered states of consciousness and technology. He discusses using VR before and after psychedelic experiences as a priming and integration tool; VR’s potential to ease first-time trip anxiety; Entheo Digital’s SoundSelf system and the powerful influence of biofeedback; and the question of whether or not technology (on its own) could initiate a non-ordinary state of consciousness with the same benefits as one brought on by psychedelics.
This episode treads lots of new ground, with Maxson discussing the likelihood of using different tools to be able to naturally activate endogenous DMT; the idea of a Steam-like internet marketplace for digital medicine; the possibility for technology to trigger lucid dreaming; the concept of highly-personalized digital schooling, and the tough question of how to not become so reliant on technology in such a quickly-advancing technological world. The challenge, which Maxson is eager to take on, is to shift opinions on VR from fear and pessimism to inspiration about what’s truly possible: How can we use technology not for escapism, but instead, for good?
“If you’re trying to drive to a yoga class, you’re usually more stressed out by the time you get there than if you hadn’t of left your house at all. And I feel like that’s the case with a lot of therapy work in general, whether it’s psychedelics or not; you could have [an] onboarding call with somebody the day before, but you have no idea what’s happening to them [in] the 24 hours leading up to them actually coming into your clinic. So I think the big focus on the priming is: how do we have reliable, very consistent treatment processes with being able to drop people into a very deep surrender, meditative, introspective state prior to them actually going into a therapeutic process?”
“I think that eventually, you’ll start to combine light, frequency, vibration, [and] electromagnetics to the point where you could actually activate DMT inside of your brain without having to use it from an external source – so like, literally using technology to activate the psychedelics inside of your own body. I think we will get to that place and that will be very interesting.”
“What [we’re] doing with creating digital medicine is a holy grail type of project, but with that comes the reverse side; which is the addiction that we already have to computers is off the charts, but what happens when you could literally press play and get high at any moment? Would people ever get off of it? So that’s a philosophical question, but I think we’re actually going to butt up against that in the next few years as we continue to develop this technology.”
“What does it look like to get in on the ground floor? It’d be really hard to do that in movies or radio or the variety of mediums; TV shows, all of those things. Like, they’re already pretty much dominated by content that we don’t really want or doesn’t make us feel better when we watch it. But with VR, it’s early enough to get in on the ground floor and create compelling alternatives to the zombie shooter games and the porn that will inevitably fill the device, and get people thinking about how to be an embodied avatar inside of a virtual world and do it for good instead of for escapism.”
Guide to Topanga Canyon: A Piece of Hippie Heaven
Truerestfranchising.com: Nick Janicki
Spiritualtechnologies.io: Don Estes
Othership.us (Robbie Bent)
Enterandromeda.com (Andromeda Entertainment)
What Technology Wants, by Kevin Kelly
The Tim Ferriss Show: Interview with Peter Thiel, Billionaire Investor and Company Creator (#28)
Reality Is Broken: Why Games Make Us Better and How They Can Change the World, by Jane McGonigal
Exploredeep.com (Deep VR)
AppliedVR.io (Applied VR)
 Lyle Maxson is the Co-Founder of GeniusX, an XR education platform reimagining online learning. He is also the Co-Founder of Andromeda Entertainment, a VR publishing company focused on bringing to market “games for good,” which developed and published the first-ever digital psychedelic, Soundself VR, as well as the breakout hit, Audio Trip (voted best dance game of 2019 by VR insider). His latest venture, Entheo Digital, seeks to provide digital therapeutics solutions for psychedelic therapy and the treatment of mental health disorders. Lyle has appeared on a variety of stages, speaking on benevolent technology and the positive impact immersive tech can play in our future. He runs a 50,000 person community of transformative entertainment enthusiasts and is a pioneer in the neurohacking movement.
Lyle Maxson is the Co-Founder of GeniusX, an XR education platform reimagining online learning. He is also the Co-Founder of Andromeda Entertainment, a VR publishing company focused on bringing to market “games for good,” which developed and published the first-ever digital psychedelic, Soundself VR, as well as the breakout hit, Audio Trip (voted best dance game of 2019 by VR insider). His latest venture, Entheo Digital, seeks to provide digital therapeutics solutions for psychedelic therapy and the treatment of mental health disorders. Lyle has appeared on a variety of stages, speaking on benevolent technology and the positive impact immersive tech can play in our future. He runs a 50,000 person community of transformative entertainment enthusiasts and is a pioneer in the neurohacking movement.



In this episode of the podcast, David interviews Anne Philippi; Founder & CEO of The New Health Club. Prior to her work with TNHC, Anne was a journalist for VOGUE, GQ, and Vanity Fair.
Philippi takes us through the arc of her departure from the media world in 2018 and into the realm of psychedelia. She opens up about her first experiences with LSD and psilocybin; how those journeys helped her shake off her “old narrative” as a journalist and step into her “real narrative”; the podcast that was birthed out of that inner work and its transformation into a business; and the work TNHC now does with ketamine and psilocybin truffles. Along with her personal story, she talks about things like integration; how the meaning of symbols witnessed in journeys becomes clearer over time; generational trauma (especially as experienced by Germans); non-linear healing; and how modern data pertaining to psychedelics is outshining the hangover from the US’s drug war propaganda.
Using the current COVID era and Ukraine/Russia conflict as examples, Philippi shares how crises can inspire togetherness and the importance of making psychedelic therapy available to refugees. She takes a very optimistic stance on the incorporation of psychedelics into the workplace as a means to help it evolve, and she talks about the toxicity of hustle culture; how safe, supported psychedelic practices can prevent burnout in the workforce; the companies that are already offering psychedelic experiences and therapy for their staff; and the value in entertaining psychedelics as a preventative measure – not just a recuperative treatment.
“I really think that with a psychedelic experience, or a regular checking in with [yourself] based on that psychedelic experience (maybe even to go on a guided trip [once or twice] a year), it’s really easier to acknowledge your body, to have a conversation with your body. Because we don’t say, ‘I’m tired, I feel like I need to take a break’; we mostly overstep that moment because then you have another coffee or you go for a run – all these tools we have in our Western society to ignore our exhaustion limits.”
“Let’s say you have an amazing psychedelic trip, and then you go back to your shitty life and you don’t change that, and you don’t go in nature, and you don’t have a community, and you’re in a toxic relationship – then the trip doesn’t actually matter in a weird way. I think that’s also something that is becoming now very clear; that the surrounding where you actually land after your trip also has to be transformed.”
“I think in the next five years, there might be completely transformed companies coming out of a psychedelic leadership idea. And again, that doesn’t mean the crazy CEO who is going crazy on ayahuasca, it’s just really to have a very conscious use of these substances, to really look into a better understanding of a very productive and creative community that is not suffering from [a] toxic work environment anymore.”
“You can find this kind of truth with the help of psychedelics. The people who I have talked to who have experienced that, whatever substance it is …pretty much, that’s the bottom line [of] what people say. At the same time, we should not really forget to say those people who found that had also done a proper integration and keep doing it, even after months and months of experiencing what they have seen.”
 Anne Philippi was a successful journalist with a strong background in established media, journalism, and communication. She published books, worked for Condé Nast, was a Vanity Fair reporter in Berlin and for GQ in Los Angeles, and she wrote for Frankfurter Allgemeine Zeitung about tech and California. In 2019, she founded The New Health Club podcast and newsletter, and created a space where CEOs, founders, investors, scientists, and therapists from the new psychedelic ecosystem and business world could talk abut the disruptive power of psychedelics, new markets, new compounds, and psychedelic medicine. In 2021, Anne made it onto Psychedelic Invest‘s list of the 100 most influential people in psychedelics. She is working on bringing The New Health Club to the next level soon.
Anne Philippi was a successful journalist with a strong background in established media, journalism, and communication. She published books, worked for Condé Nast, was a Vanity Fair reporter in Berlin and for GQ in Los Angeles, and she wrote for Frankfurter Allgemeine Zeitung about tech and California. In 2019, she founded The New Health Club podcast and newsletter, and created a space where CEOs, founders, investors, scientists, and therapists from the new psychedelic ecosystem and business world could talk abut the disruptive power of psychedelics, new markets, new compounds, and psychedelic medicine. In 2021, Anne made it onto Psychedelic Invest‘s list of the 100 most influential people in psychedelics. She is working on bringing The New Health Club to the next level soon.
Socials: Instagram / Twitter / LinkedIn



In this episode of the podcast, recorded live from the Archipelago Attic space in Denver, CO, Joe sat down with Unlimited Sciences founder, Del Jolly; Former UFC champion and Hall of Famer, Rashad Evans; and 10-year NFL veteran quarterback, Jake Plummer, at the initial launch of their new functional mushrooms company, Umbo Mushrooms.
Plummer and Evans tell their story of how they met Jolly and transformed from professional athletes to long-haired mycophiles who are now running their own mushroom company; discussing how difficult transitioning back to normal everyday life after a sports career can be, and how CBD, following the Stamet’s stack protocol, and learning about all the anecdotal evidence of brain injury healing started to make them question what kind of long-term issues they may have coming to them (fellow athletes have asked Evans: “Do you feel it?”). Jolly believes that functional mushrooms have just as much, if not more potential to help humanity than the often higher-praised psilocybin.
The four of them talk about a lot more in this nearly 2-hour panel discussion (with audience questions): the power in language and how a diagnosis can be a wall people put up that blocks progress; how valuable it is to learn from each other in group preparation and integration sessions (Evans calls these ceremonies “share-emonies” for this reason); how the UFC and NFL feel about psychedelics; microdosing and competition; NFTs; the Telluride Mushroom Festival; and the problem with TBI often being misdiagnosed as PTSD. And they discuss what steps we can take to better align our communities to the set and setting we want; the importance of slowing down; how every person has a specific audience they can reach; how we can learn from Indigenous people about our lost connection to community; and the interesting question of if we actually feel better from eating mushrooms because as a society, we completely removed them from our diets and our bodies have been craving them ever since.
Umbo Mushrooms has just recently launched and they’re offering a 20% off discount for PT listeners (use code Unlimited20 at checkout). Additionally, if you are planning to use psilocybin outside a research laboratory before July 1st, Unlimited Sciences is running a study to learn more about the positive and/or negative outcomes of using psilocybin in more natural settings. You can participate here.
“As a big advocate for psilocybin in particular, functional mushrooms have just as much, if not more potential to help humanity than psilocybin. I really believe that. And it’s just a matter of time before some eight year old kid is going to come up and say, ‘Oh, that’s the key. Look what I found!’ Boom. ‘Now my Dad really isn’t going to age.’” -Del
“I think tapping into those Indigenous voices – those stories, the history – is very important for the movement because they understood community. And when you look at what are the biggest [ailments] in our society is the fact that we have a broken community. Our communities are broken for the larger part. And finding ways to tap back into that old knowledge of ways we used to be can get us to remember what we are [and] how to be towards each other. I think that we don’t get better as a world until we get better as a community, and I think tapping into those strong Indigenous community roots would help us to be what we could be.” -Rashad
“The world doesn’t need psychedelics. The world needs community and a meditation practice. But psychedelics is the 2×4 that brings you to that awareness.” -Del
“Don’t minimize what your impact is. If you’re Rashad Evans with a platform, [a] Hall of Famer, Jake Plummer, [whoever]… Either you’re that or this. Don’t minimize what it is, because whoever you’re speaking to might be the person who sets it off.” -Del
“I think once you get into the mushrooms, you can’t help but learn more kindness, compassion, and love. It will open your mind. That’s kind of why I said those three words; is if we can keep that in front of everything and also the sacred part of everything… Everything should be a lot more sacred than it is, everything we do. I find myself grabbing food and eating it and then going, ‘Damn, I didn’t even really thank this food for being here.’ We take a lot of things for granted, so I think just starting with that awareness can be a step in the right direction.” -Jake
Unlimitedsciences.org: Real-world psilocybin mushroom study
Psychedelics Today: Del Jolly – Psilocybin, Concussions, and Unlimited Sciences’ Mission
Ffungi.org (The Fungi Foundation)
Microdosinginstitute.com: Stamets Stack
YouTube: Joe Rogan Experience #1035 – Paul Stamets
Mushroomdesign.com: How (and why) cordyceps were mistaken for steroids in the 1993 Olympic Games
YouTube: “When The Bright Lights Fade”
Psychedelics Today: PT246 – Amber and Marcus Capone of VETS – Foundational Healing and the Brain
Metatoadsgang.io (Rashad Evans’ NFT project)
The More Beautiful World Our Hearts Know Is Possible, by Charles Eisenstein
Archipelagodenver.com (where this podcast was recorded)
 Del Jolly (right) is a Co-Founder of Umbo Mushrooms and Co-Founder of Unlimited Sciences, a psychedelic research non-profit.
Del Jolly (right) is a Co-Founder of Umbo Mushrooms and Co-Founder of Unlimited Sciences, a psychedelic research non-profit.
Instagram / Twitter / Facebook
“Suga” Rashad Evans (left) is a former UFC light heavy weight champion and Hall of Famer. He currently is an ESPN analyst for the UFC and Co-Founder of Umbo Mushrooms.
Instagram / Twitter / Facebook
Jake Plummer (center) is a former NFL Pro-bowl quarter back who played 10 years in the league with the Arizona Cardinals and the Denver Broncos. He is now a mycophile who runs Umbo and Mycolove Farms.



In this episode of Vital Psychedelic Conversations, Kyle interviews Daniel McQueen, MA: psychedelic specialist, educator, and author of Psychedelic Cannabis: Therapeutic Methods and Unique Blends to Treat Trauma and Transform Consciousness. McQueen is the Executive Director of the Center for Medicinal Mindfulness in Boulder, CO, where he facilitates psychedelic sessions with cannabis and ketamine.
This talk covers a lot but really hits home on a few very important topics: the clinical model’s limited perspective; the importance for psychedelic boards to self-organize before government agencies step in; and how cannabis can actually be as powerful a psychedelic as DMT. They mull over where the field of psychedelics is going and wonder: Who gets to do this work? And can psychedelics really fit within our current medical models?
McQueen digs into the non-licensed approach to facilitation; the difference between coaching, counseling, and psychotherapy; and describes valuable harm reduction strategies, vital self-care practices for facilitators, and ways to navigate the (not talked about enough) transformational process of being a guide for others. If you experience anxiety or paranoia from cannabis, you’ll learn how Nano CBD can shut it down almost instantaneously. Last but certainly not least, McQueen shares all about the transformative work and trainings he and his colleagues are doing at both the Center for Medicinal Mindfulness and Psychedelic Sitters School.
“We’ve got to have our boards, we’ve got to become members of those boards, and we’ve got to self-organize and regulate. Otherwise, the government agencies are going to do it for us. It’s going to become super clinical, super medical. It’s going to limit the scope to only people who are really suffering and I think that’s a trap.”
“I’m thinking [cannabis is] probably one of the best psychedelics for trauma resolution work and other things. So I’m way past ‘Is this psychedelic?’ I’m stepping into: ‘This might be one of the best medicines for psychedelic therapy and guiding that we have available.’”
“I just was intuitively drawn from the beginning to do blends – to blend multiple strains [of cannabis] together – and I started to experiment on my friends. …One of my friends …sat up and said, ‘Daniel, if I didn’t trust you, I would swear you put DMT in that.’ And I hadn’t, it was just pot. And that was the moment. I’m like, ‘Okay, maybe there’s something to this.’”
“Sometimes these stories that we hear are the hardest stories to hear from another human being. So there’s an emotional impact to process. I’ve had to really evaluate my existential understanding of reality because of this job, so there’s that whole thing too. It’s not the same as psychotherapy, it’s just not. Professionally speaking, I tell people it’s more like being an emergency medicine doctor. You’ve got to take time off. Self-care is vital.”
Psychedelics Today: Daniel McQueen – DMTx and Future Psychedelic Technologies
Psychedelics Today: Daniel McQueen – Extended-State DMT Research (DMTx)
Psychedelics Today: Daniel McQueen – Medicinal Mindfulness & Conscious Cannabis Circles
Psychedeliceducationcenter.com: DMTx Psychonaut Training Webinar
Naropa.edu: Psychedelic-Assisted Therapies Certificate
Dr. Michael Harner: The Foundation for Shamanic Studies
 Daniel McQueen, MA, is a psychedelic specialist, educator, and author of the book, Psychedelic Cannabis: Therapeutic Methods and Unique Blends to Treat Trauma and Transform Consciousness. In 2012, he co-founded one of the first legal psychedelic plant medicine therapy clinics in the United States, the Center for Medicinal Mindfulness, which is located in Boulder, Colorado, and is currently celebrating its 10-year anniversary. The same year, Daniel also founded Psychedelic Sitters School, which continues to train students from around the world in mindfulness-based psychedelic therapy and cannabis-assisted psychedelic therapy.
Daniel McQueen, MA, is a psychedelic specialist, educator, and author of the book, Psychedelic Cannabis: Therapeutic Methods and Unique Blends to Treat Trauma and Transform Consciousness. In 2012, he co-founded one of the first legal psychedelic plant medicine therapy clinics in the United States, the Center for Medicinal Mindfulness, which is located in Boulder, Colorado, and is currently celebrating its 10-year anniversary. The same year, Daniel also founded Psychedelic Sitters School, which continues to train students from around the world in mindfulness-based psychedelic therapy and cannabis-assisted psychedelic therapy.
Socials: Instagram / Twitter / Facebook



In this episode of the podcast, Joe interviews Licensed Chemical Dependency Counselor and Holotropic Breathwork® facilitator, Christine Calvert.
At age 19, Calvert left Los Angeles and found her way to breathwork, spending four years in Grof Transpersonal Training. She quickly discovered that the technique served as a gateway back home to herself – her sacred self. Together, Christine and Joe cut through the many layers of the holotropic paradigm and transpersonal experiences, discussing how willingness for accountability & repair in facilitation are more important than perfection; the role of touch in breathwork sessions and the potential harm in not providing it; how amplification over suppression of symptoms in breathwork can heal; and how doing less as a facilitator can actually do more.
She also talks about the inner healing intelligence we all possess; how celestial nostalgia leads to mystical yearning; the ethics of spaceholding; the excitement and terror in expanded states of consciousness; saying yes to the entire archetypal pool; how Grof was (and still is) decades ahead of psychology; and what it means to die to ourselves.
“There [were], I don’t know, 175 people there. So that was my first big group breathwork. I was sitting first and I remember just looking out at the room which was just absolute pandemonium. It was like the display of the full human experience. I remember just crying because I was both totally intrigued and excited – like ‘Finally, I’ve arrived’ – and then I was also just incredibly terrified. I feel like that’s an interesting and kind of truthful reflection of how expanded state work is for a lot of people. There’s this part of me that feels home and also maybe a little healthy resistance to knowing what that also means for me.”
“One of the greatest gifts we can do for someone is to trust that what is happening for them is exactly what is needing to come through for their healing and that there’s nothing that we necessarily need to do in order to manage that.”
“I can’t imagine that continuing to just treat symptoms and see everything through a pathological lens is really all that fulfilling. Also we’re just the doers in that world. And as much as I think our ego wants that, behind that is always the desire to be a part of something that’s actually truly healing, and to know that we’ve empowered somebody to heal themselves. This is one of the things I love so much about the holotropic paradigm; is that it is about radical self-empowerment.”
“I think we have to stop being afraid to just be vulnerable. We have to stop being afraid of our humanity. As facilitators, as practitioners, as spaceholders, as participants in medicine and breathwork – this is what we have to really be willing to share. …When we’re willing to sort of knock ourselves off the saint pedestal as facilitators and spaceholders, I think then we might be able to hold this.”
Holotropic.com: Grof Transpersonal Training
The Ethics of Caring: Finding Right Relationship With Clients, by Kylea Taylor
Exploring Holotropic Breathwork, Edited by Kylea Taylor
 Christine Calvert is a teacher and module facilitator for Grof Transpersonal Training and a Licensed Chemical Dependency Counselor. In addition to bringing Holotropic Breathwork® and other experiential workshops to mental health and addiction facilities, she is passionate about the ethics and integrity needed in facilitating expanded-state work; supporting the integration of Holotropic and psychedelic sessions through somatic resourcing; and creative expression, personal ritual, and group support. Her own personal healing journey was greatly influenced by the Holotropic perspective and she feels deeply dedicated to sharing this work with those seeking healing. She enjoys finding ways to weave her personal and professional experience of different therapeutic and spiritual systems such as Shamanism, Somatic Experiencing, Jungian psychology, attachment theory, and mindfulness practices into her work with others. Christine is currently studying to become a Naturopathic Doctor and maintains a private counseling and consulting practice in addition to facilitating Holotropic Breathwork® nationally.
Christine Calvert is a teacher and module facilitator for Grof Transpersonal Training and a Licensed Chemical Dependency Counselor. In addition to bringing Holotropic Breathwork® and other experiential workshops to mental health and addiction facilities, she is passionate about the ethics and integrity needed in facilitating expanded-state work; supporting the integration of Holotropic and psychedelic sessions through somatic resourcing; and creative expression, personal ritual, and group support. Her own personal healing journey was greatly influenced by the Holotropic perspective and she feels deeply dedicated to sharing this work with those seeking healing. She enjoys finding ways to weave her personal and professional experience of different therapeutic and spiritual systems such as Shamanism, Somatic Experiencing, Jungian psychology, attachment theory, and mindfulness practices into her work with others. Christine is currently studying to become a Naturopathic Doctor and maintains a private counseling and consulting practice in addition to facilitating Holotropic Breathwork® nationally.



For our first ever Earth Day episode, Joe interviews publisher, ecologist, and planetary steward, Deborah Snyder. Snyder is the co-owner of Synergetic Press and its associated organic farm, orchard, and retreat center, Synergia Ranch.
Snyder worked with the team that designed and built Biosphere 2, and she unpacks the many ways in which understanding the planet as a biosphere – a collection of cooperative living systems – can shift our perspectives and help us to heal our precious home. She discusses how monitoring the earth from space can teach us how best to care for it; the technosphere’s disharmonious relationship with the biosphere; the anthropocene epoch; Synergia Ranch and Synergetic Press; the importance of recognizing ourselves as an integral part of nature; and the ways psychedelic and ecological spaces overlap. While both agree that the environment is in trouble, they have an air of optimism and action that we all desperately need in order to secure the future of the planet and our species.
This episode also features a brief chat between Joe and Kyle, with Joe calling in from Bicycle Day San Francisco. With Vital officially launching the same week we hit 3 million downloads of the podcast (!!!), they felt it was worth doing a rundown of the top 8 most downloaded episodes, as well as highlighting some of their favorites. Thank you to everyone who has been listening and sharing your favorite episodes with friends. To 3 million more!
“I would describe the psychedelic world as tools to be able to enhance a person’s ability to explore and to understand what connections and interrelationships are. Many people that have had grand epiphanies that have led to whole new revolutionary technologies attest to this phenomenon. So Biosphere 2 was definitely an example of the creativity that came out of people that were able to do that.”
“We are very much nature and I think that we need to really work on our value of what that brings us and carefully consider before utilizing those resources for something that is perhaps just a one-way street.”
“I have never met anybody that has undergone or gone through any kind of transformative experience for themselves or looking for insight that hasn’t come out with a greater appreciation for the nature of which we are a part.”
Psychedelics Today: PT228 – Deborah Snyder from Synergetic Press
The United States Environmental Protection Agency (EPA)
Wikipedia.org: Vladimir Vernadsky
Wikipedia.org: Anthropocene Epoch
Tamera.org: Peace Research & Education Center
Vandana Shiva | Synergetic Press
The Rose of Paracelsus: On Secrets & Sacraments, by William Leonard Pickard
LSD My Problem Child: Reflections on Sacred Drugs, Mysticism, and Science, by Albert Hofmann, Ph.D.
LSD Psychotherapy: The Healing Potential of Psychedelic Medicine, by Stanislav Grof
 Deborah Snyder, co-owner and publisher of Synergetic Press, Ltd., has published over 40 books in ethnobotany, psychedelics, biospherics, consciousness, and cultures since establishing it in 1984. In 1986, she was on the team that designed and built Biosphere 2. There, she met Richard Evans Schultes, publishing his two classic books on ethnobotany of the Colombian Amazonia. In 1990, she started The Biosphere Press, an imprint of Space Biospheres Ventures, producing a dozen books for children on biospheres and biomes; developed a K-12 curriculum; and helped launch the first peer-reviewed journal in closed ecological systems, Life Support and Biosphere Science. In 1999, she moved to Synergia Ranch, in Santa Fe, NM, which was established in 1969 as an intentional community and site where the Institute of Ecotechnics formed. Deborah is currently a director and VP of the U.S. non-profit. Synergia Ranch is home to a 4 acre organic orchard, a half acre market garden, and small retreat center. From 1982 to 2019, Deborah spent time volunteering most years on the Institute’s pastoral regeneration project in the northwest Kimberley of West Australia. Starting as an apprentice in savannah system management, by 1990, she became a co-owner and chairwoman of the 5000 acre freehold property). A recent documentary, “Spaceship Earth,” features the work of the Institute and its landmark ecological project, Biosphere 2. Click here for a short video on how Deborah got into publishing and her relationship with Ecotechnics on City Lights Bookstore’s Youtube channel.
Deborah Snyder, co-owner and publisher of Synergetic Press, Ltd., has published over 40 books in ethnobotany, psychedelics, biospherics, consciousness, and cultures since establishing it in 1984. In 1986, she was on the team that designed and built Biosphere 2. There, she met Richard Evans Schultes, publishing his two classic books on ethnobotany of the Colombian Amazonia. In 1990, she started The Biosphere Press, an imprint of Space Biospheres Ventures, producing a dozen books for children on biospheres and biomes; developed a K-12 curriculum; and helped launch the first peer-reviewed journal in closed ecological systems, Life Support and Biosphere Science. In 1999, she moved to Synergia Ranch, in Santa Fe, NM, which was established in 1969 as an intentional community and site where the Institute of Ecotechnics formed. Deborah is currently a director and VP of the U.S. non-profit. Synergia Ranch is home to a 4 acre organic orchard, a half acre market garden, and small retreat center. From 1982 to 2019, Deborah spent time volunteering most years on the Institute’s pastoral regeneration project in the northwest Kimberley of West Australia. Starting as an apprentice in savannah system management, by 1990, she became a co-owner and chairwoman of the 5000 acre freehold property). A recent documentary, “Spaceship Earth,” features the work of the Institute and its landmark ecological project, Biosphere 2. Click here for a short video on how Deborah got into publishing and her relationship with Ecotechnics on City Lights Bookstore’s Youtube channel.



In this episode of Vital Psychedelic Conversations, David interviews Omar Thomas: Founder of Jamaica’s Diaspora Psychedelic Society, CEO of Jamaican Organics, Psychedelics Today Advisory Board member, organic farmer, and certified death doula.
Thomas discusses how we define home, the importance of having open dialogue with our children about psychedelics, how the psychedelic experience relates to permaculture, our cultural absence of a rite of passage, the joy in psychedelics, and the value in allowing change to become a natural evolution we experience once we take the mindful seat of the observer.
Thomas breaks down all the ways in which Jamaica is shaping its framework as a psychedelic-informed health & wellness destination and the country’s cultural roadblocks that could potentially impede its development. And he talks a lot about his work as a death doula: the importance of taking a more sacred and preparatory approach to death, how helping someone through the transition is the ultimate holding of space, and how each psychedelic trip can be a practice session for death.
A theme that is consistent throughout this conversation is self-directed growth via The Warrior’s Way – an exercise in discovery, surrender, and developing daily practices toward change. Thomas posits that it’s when we hold space and shed the many layers of our identity that we can begin to foster real change – by “staying on” and becoming an observer rather than directly trying to change things, change will happen naturally.
“The things you need for a psychedelic trip are the same things you need for life. You need courage when you’re afraid and you need to prepare yourself for the things you’re going to undertake, and to do them seriously and with appreciation for the moment.”
“The idea of holding space is so much about us not being in the way of hearing what others have to say, and allowing them to come to realizations that they would come to naturally if they would but take the time to sit for a while and contemplate the idea without distraction.”
“I found that Jamaica itself is healing. The island is healing. And I don’t want to get too esoteric about it, but there’s something about even just being outside for me in the early morning hours before the sun rises in a climate that can allow me to do so comfortably, and to be able to start to appreciate still connection, just on its own – I’m finding that this place seems to be tuned to some sort of frequency. It just makes it easier to slip into a feeling of wholeness, or at least of wanting to be.”
“We have our lifetimes only to begin to affect the change in the things that move us. If we are upset about the climate, let’s use the life we have. Let’s use the life we have to connect so that when death comes, we have lived a life worth living, that’s so satisfying that it’s okay to let go. For me, the psychedelic trip and journey is about letting go in a micro sort of way. Each trip is a practice session.”
“I’ve seen people laugh and chuckle now at the idea of not being, because during the trip, they learned that there’s no way to not be, because matter cannot be created or destroyed. …We’re afraid of smoke and mirrors and shadowboxing – things that we don’t need to fear.”
 Omar Thomas is the founding advisor of Diaspora Psychedelic Society (DPS) and a member of the Jamaican Diaspora Task Force on Behavioral Health. His Afro-Caribbean upbringing led him to seek out non-traditional answers to his own PTSD and trauma issues in the early 90s. His search eventually took him to Mexico where he underwent 30 days of fasting, isolation, and intensive sacred mushroom work under curandero guidance. He’s lived as a permanent resident of Mexico for a number of years developing a deeper connection to the medicine in the context of community. He brings his years of experience in Mexico to bear in guiding the vision for DPS.
Omar Thomas is the founding advisor of Diaspora Psychedelic Society (DPS) and a member of the Jamaican Diaspora Task Force on Behavioral Health. His Afro-Caribbean upbringing led him to seek out non-traditional answers to his own PTSD and trauma issues in the early 90s. His search eventually took him to Mexico where he underwent 30 days of fasting, isolation, and intensive sacred mushroom work under curandero guidance. He’s lived as a permanent resident of Mexico for a number of years developing a deeper connection to the medicine in the context of community. He brings his years of experience in Mexico to bear in guiding the vision for DPS.
Through Diaspora Psychedelic Society, Omar collaborates with a number of organizations to promote more equitable access, Jamaican inclusion, and innovative approaches to psilocybin-supported therapies. In addition to overseeing day-to-day DPS activities, he is the CEO of Jamaican Organics, and sits on the strategic advisory board of Psychedelics Today.
Omar now resides on his ancestral island home in St. Elizabeth, Jamaica.
Diaspora Psychedelic Society socials: Instagram / Facebook



The continued exploitation of this fragile species for its DMT encapsulates narcissism itself.
Until recently, the Sonoran desert toad, Incilius alvarius (formerly Bufo alvarius) was not on my wildlife-watch radar. Then an email from the owner of a group of psychedelic retreat centers operating in Latin America, Portugal, and the Netherlands brought the greenish brownish warty native of the Sonoran desert to my attention. He was writing to let me know that the personality disorder of narcissism, the toxic world-killer which has brought life on Earth to an environmental and climatological precipice, could be cured – with psychedelics. Specifically with “Toad Venom.”
“With expert guidance and facilitation, psychedelics can help us… be collectively healthy, happy, and harmonious in the stewardship of our planet,” he wrote.
Curious, I clicked on a link for a “Transformational Bufo Alvarius Retreat (5-MeO-DMT, Toad Venom).” According to the ad, “5-MeO-DMT, also known as the sacred toad medicine, is a beautiful teacher that can lead to profound transformation when facilitated by experienced guides,” and they would be offering dimethyltryptamine (DMT) in its 5-MeO-DMT – toad form – as the chemically mediated gateway to this process.
As something of an expert in identifying displays of cognitive dissonance, the suggestion that exploiting a toad in the interest of curing Homo sapiens of his most reprehensible trait was not sneaking past my cognitive threshold.
I love amphibians. I always have. When I lived in Kenya as a teenager, the red legged Hyperolius viridiflavus flashed from reed to reed in the dam below the house; on a trip to Madagascar, I observed the tomato frog, Dyscophys antongilii, sequestered in a storm drain in a village; near my former home in the Sierra Nevadas, the mountain yellow-legged frog, Rana muscosa chirped in mountain lakes every spring.
Worldwide, amphibians are the most threatened class of vertebrates on the planet. Although thought to be abundant in its home range of the Mexican state of Sonora and parts of Arizona, the Sonoran desert toad is on endangered species lists in both California and New Mexico. In Arizona, a fishing license grants collection of up to ten live Sonoran toads. Shipping them to another state or abroad is illegal and prosecutable, as is possession of the psychedelic 5-MeO-DMT.
Prohibition against toad possession has not stopped poachers though. In Arizona, poachers were caught on camera dumping toads into plastic bags in a wildlife conservation area.
Increased toad poaching and illegal transport across state borders and the US-Mexico border has recently triggered the Lacey Act, which prohibits import, export, sale, acquisition or purchase of fish, wildlife or plants transported, or sold in violation of US, Indian or international law. Law enforcement agents for the US Fish and Wildlife Service (USFWS) confirmed they are currently carrying out an investigation. Whether their efforts are successful in reducing illegal trade remains to be seen.

DMT is a trace neurotransmitter found in mammalian lungs and brains, as well as in numerous plant species. The DMT molecule was first synthesized in a lab in 1931 by Canadian chemist, Richard Manske. Its natural occurrence in plants was not confirmed in Western science until microbiologist Oswaldo Gonçalves de Lima did a biochemical study of Mimosa hostilis in 1946 after observing the Indigenous Pancuro Tacarutu (Brazil) ceremonially drinking an intoxicating brew* called vinho da jurema distilled from the plant’s root bark. In 1956, Hungarian chemist and psychiatrist, Stephen Szara extracted DMT from Mimosa hostilis, gave himself an intramuscular injection of it, and experienced a “psychotic effect to the serotonin metabolism.”
The now discredited hypothesis that Indigenous groups used a hallucinogenic compound derived from toads was put forth by anthropologist Dr. Jeannette Runquist, and reported in a 1981 issue of Omni Magazine. She described decapitated toad skeletons buried near excavations of ancient Cherokee encampments in North Carolina, and wrongly inferred that what was, in fact, food waste as the telltale sign of Indigenous mysticism.
“Food trash was taken for psychedelic magic,” said Robert Villa, Research Associate, Tumamoc Desert Laboratory, Tucson, Arizona, and President of the Tucson Herpetological Society. “Toads were skinned and eaten as survival food, as part of the ordinary diet.”
Despite claims on the part of modern healers, there is no evidence in the archeological record of toads being used ceremonially by Indigenous groups in the Americas.
“For such a significant smoke, there would have to be some record of it,” said Mr. Villa. “Even though Indigenous cultures can be good at hiding things from outside inquisition, this is too significant to go unnoticed,” he said. “The significance of the toad in Indigenous culture isn’t what people want to believe,” said Mr. Villa. One of his goals is “to stop the appropriation of Indigenous culture around the Sonoran desert toad. All of the archeological leads are dead ends.” Using the abundant depictions of toads in Mesoamerican culture to bolster the specious claim that the toads were used in psychedelic rituals represents cultural hijacking.

For ancient cultures, the life cycle of the Sonoran toad embodied rebirth and renewal. Its seasonal appearance – they spend ten months of the year underground, emerging briefly in July and August during the rainy season to mate and reproduce – as well as its complex life cycle, which involves metamorphosis from a water-dwelling, gill-breathing, fish-like tadpole to land-dwelling, four-legged adult toad adds to its supernatural aura.
“They were thought to interact with gods of the underworld,” said Mr. Villa. In Sonora, locals avoid them as toxic. Among the Indigenous groups in northern Mexico, their appearance is associated with the arrival of seasonal rains. Disturbing them is an accursed act which can disrupt weather patterns. “You could incur damages from the gods in the form of drought or flooding if you harass a toad,” he said.
The evidence, according to Mr. Villa and other scientists who have explored the natural history of Incilius alvarius, indicates extracting and smoking toad-derived 5-MeO-DMT is a post-industrial phenomenon. It has nothing to do with cultural tradition. In recent years, however, “smoking toad” has become the new psychedelic fad, making Incilius alvarius the latest must-have in the growing list of psychedelic consumables. And in response to increasing demand from the tourism and retreat industries, one Mexican coastal group whose members have subsisted on tourism – mostly selling ironwood carvings to foreigners – have begun peddling Sonoran toad medicine to foreigners.
“The Seri, or Comcaac [an Indigenous group living on the mainland coast of the Gulf of California] adopted toad magic and medicine as a tourism item. They’re trying to make a living by facilitating people smoking this stuff. It’s not part of their history,” said Mr. Villa.
There is hearsay evidence, according to Mr. Villa, that regional cartels have begun exploiting this practice as well, as further means to extort locals in the interest of serving what is becoming a global trade.
The entry of toad medicine into modern psychedelia is itself a twisted tale. Back in 1981, the Omni article piqued the interest of one reclusive resident of Denton, Texas, named Ken Nelson. While studying at the University of North Texas, Mr. Nelson commenced an earnest inquiry into toad skin secretions. He came across the work of the Italian toxicologist Dr. Vittorio Erspamer, whose most important contribution to neuroscience was the identification and synthesis of the neurotransmitter, serotonin. As a toxicologist, Dr. Erspamer was most interested in the exudate from amphibian parotid glands as a possible source of new medical drugs. His chemical analysis of the venom from 40 toad species serendipitously yielded the finding Nelson had hoped for: one species, Incilius alvarius synthesized a DMT-containing substance. Mr. Nelson documented his discovery and techniques for extracting, drying and smoking 5-MeO-DMT in his 1984 pamphlet: “Bufo alvarius: the Psychedelic Toad of the Sonoran Desert,” which he published privately under the pseudonym, Albert Most.**
Unwittingly, Mr. Nelson opened a Pandora’s box. Since then, a fabricated sacred mysticism has evolved around Incilius alvarius and the DMT squeezed from its glands. Despite the explicit wishes of Mr. Nelson, an ardent conservationist, who towards the end of his life expressed concerns about the ecological repercussions from misrepresentation of his work, use of 5-MeO-DMT has skyrocketed in recent years. Even though DMT can be fabricated in a lab with legal, commercially available chemical precursors, many practitioners – such as the retreat proprietor – adhere to a new age belief that there is something mystically special about DMT extracted from live toads.
I questioned the proprietor of the psychedelic retreat about the authenticity of his claims about 5-MeO-DMT. Why could he not use the lab-formulated version? Endangering the life of a wild animal in order to cure narcissism did not jive with his stated intentions. This fat little toad about the size of my hand was the embodiment of nature itself; and yet he as a Caucasian, self-styled psychedelic healer was exploiting it as a commodity. The toad had no say in its own destiny.
The proprietor responded by invoking an unknowable mystical consciousness with which he and his associates – the people responsible for collecting toad venom – were imbued. “We know what we are doing is for the good of humankind, in keeping with the sacred spirit of those who have preceded [us] in this practice,” he said. Those who collect the toad, he said, are performing a consecrated task. One of his practitioners, a Swedish man who guides DMT sessions at his retreats, described collection and use of the toad as a sacrament: “I only order [5-MeO-DMT] through sources I know,” he said. “It’s energy medicine, so the energy has to be right.” The source, he said, was a Mexican friend who has tribal connections and harvests the medicine directly. He would never use toads gathered the way he’d seen in videos – en masse and thrown in garbage bags.
“My sources milk toads once a year. They do it with respect and prayers. They put the toads back in the same location. They mark the toads so they don’t milk them several times.” Safety and purity, he said, were of the utmost importance.
Knowing what I know, the invocation of sacred ancestral spirits looked a lot like chicanery. The toad was the prima facie victim of narcissism.
Identification with the Divine as a way to aggrandize oneself out of personal responsibility is, unfortunately, an all-too-common maneuver in psychedelic circles. This reflexive hopscotch affords participants the luxury of justifying anything they do: their particular psychedelic experiences are so sacred and important, normal rules do not apply. Any rules, all rules – whether psychological, medical, scientific, or ethical.
“Piaget’s concepts of schema and assimilation (vs. accommodation) seem relevant for understanding many of the less desirable potential outcomes of psychedelic use, including worsened narcissism, spiritual bypassing, guruism, unethical business practice, and bad music taste,” noted psychotherapist Max Wolff wryly in a tweet.
Assimilation occurs when we modify received information to fit with our existing knowledge and assumptions. Accommodation occurs when we reshape our perceptions in response to problems posed by the environment. We restructure what we already know so that new information can enter our universes. In the psychedelic space, real learning is so rare it is nothing short of miraculous. Most of the time, psychedelic experiences are no more transformative than a day trip to Disneyland.
Although practitioners and hobbyists argue they don’t harm the toad when they milk its glands, Mr. Villa points out toads are harmed when they are handled and moved; and collecting and transporting the toads is tantamount to killing them. “They’re very territorial,” he said. “Imagine if someone picked you from your house, put you in a sack and then moved you to the Saudi Arabian desert and left you there. Would you survive? Would you know how to get home?”
The biggest impediment to toad conservation, said Mr. Villa, is the absence of real population data. “To identify the problem, we have to have a snapshot of the past, a baseline. We don’t have that.”
The toad’s life cycle itself presents a challenge to population assessment. For most of the year, mature adults live underground in a quiescent state. They emerge when it starts raining, and there’s a breeding frenzy. Adult toads are conspicuous for about a month, then they go underground again. Tadpoles can be seen swimming in surface ponds until they mature. If there’s a lengthy drought, the subterranean toads survive in a state of something like suspended animation for years, making live populations hard to count. Years can pass when very few are observed. A rainstorm, and there are thousands where there were none.
“We think they live a long time,” said Thomas R. Jones, Ph.D., Amphibians and Reptiles Program Manager for the Arizona Department of Game and Fish. “We don’t think three or even more years of poor rainfall affects the toads. They persist. When it finally rains, they come back out again,” he said.
The Arizona Department of Game and Fish has been monitoring a population at one site, but the data don’t account for the toads’ vast range, which stretches from the Sonoran desert in northern Mexico through Arizona and parts of New Mexico. Climate change, habitat destruction, and increased poaching add further obstacles. A local population in southeastern California was extirpated decades ago. None have been observed since the 1970s.

Counting their numbers does not address the fundamental problem with exploiting the toads, though, as reducing an amphibian member of the Sonoran desert ecosystem into raw material in service of a global supply chain is a moral travesty.
“Solutions most people conceive of as viable are implicitly biased by capitalism,” said Mr. Villa. “You might hear: ‘We’ll just breed them in captivity.’ In Hungary, there’s a small-scale operator doing it. Most captive breeding programs fail in some way.” There’s the problem of crowding, of waste water contamination, and of the captive animals becoming reservoirs for amphibian diseases like chytrid. The idea of breeding something to exploit is itself repugnant to Mr. Villa.
“There are more cogs than people really understand when it comes to this,” said Mr. Villa. “Few people have the ability to contemplate whether what they’re consuming is directly exploiting Indigenous people or an ecosystem. Does someone smoking 5-MeO-DMT in an east coast city consider whether they’re directly or indirectly exploiting someone down the supply chain?”
Chemists who formulate DMT have concluded there is no qualitative difference between psychedelic trips using the lab-made product and 5-MeO-DMT extracted from the toad’s parotid gland. Although the argument has been made that other compounds such as bufotenine, another tryptamine psychedelic found in low concentrations in some toad secretions, can contribute a certain je ne sais quoi to the experience, repeated testing of Incilius alvarius secretions yielded negligible bufotenine concentrations. There is no entourage effect. Furthermore, chemically and metabolically, formulated DMT is far purer. Samples of the dried toad secretion typically contain about 30 percent 5-MeO-DMT by mass. The remaining 70 percent is composed mostly of salts, proteins, and other high molecular weight chemicals. In other words, it’s saliva.
To suggest there’s anything special about 5-MeO-DMT flouts an established, well-respected component of the psychedelic tradition. More than any other factor, the subject’s own mindset – part of the psychedelic “set and setting” equation – determines how the trip goes.
5-MeO-DMT extracted from Incilius alvarius won’t cure narcissism. Projecting our spiritual expectations onto a toad only harms the toad.
*Goncalves de Lima, O. (1946). Observacio es sobre o “vinho de Jurema” utilizado pelos indios Pancaru’ de Tacaratu’ (Pernambuco) [Observations on the “vinho de Jurema” used by the Pancaru’ Indians of Tacaratu’ (Pernambuco)]. Ariquivos do Instituto de Pesquisas Agronomicas, 4, 45–80.
**Most, Albert. Bufo alvarius: the Psychedelic Toad of the Sonoran Desert. 1984; updated 2020. Venom Press. Denton, Texas. The 2020 updated edition contains detailed instructions for synthesizing DMT in a lab.
In this episode of Vital Psychedelic Conversations, Kyle interviews clinical psychologist and integration facilitator (and now 3-time guest), Dr. Ido Cohen.
The topic of integration sits center stage for this discussion, as the two peel back all the nitty gritty and nuance of this psychedelic cornerstone, breaking down why integration is so important, where it stands currently, and where it needs to go as psychedelic-assisted therapy grows. They discuss the importance of taking it slow when it comes to exploration of these non-ordinary states – something that can be so difficult for us in our fast-tracked, clock-watching, Western culture, where it’s quite common for people to get blasted into inner-space on a Saturday, be shaken and perplexed by the experience on Sunday, and then have to go back to work and act like it never happened by Monday.
He discusses the value that both individual and group integration holds; what happens when you sit in groups of the same people over time; why Carl Jung never tried psychedelics; and the importance of tolerance, trust, and critical thinking when processing peak experiences.
And he raises some important questions like: What does long-term care in psychedelic-assisted therapy look like? What frameworks can be experimented with and implemented now to offer real movement from peak experiences to sustainable change? What is that bridge between peak experience and long-lasting change which allows us to become the insight? Is every insight true? Where does trauma work fit into this treatment? And what is the difference between symptom reduction and real healing?
“My mission has been: what does that bridge [look like] between experience and the steps that we have to take to really integrate in a deep embodied way to move from, ‘Oh, I can become this thing’ or ‘I have this insight’ to becoming the insight or becoming the thing?”
“I always use this catchphrase because I don’t like it, but it sells the psychedelic science: ten years of therapy in one session. I always say if you get ten years of therapy in one psychedelic session, then you had really bad therapy.”
“The psyche has an organic life. It opens up in the way it opens up. You can bathe yourself in ayahuasca and eat fifty grams of mushrooms per week [but] there are certain processes you can’t rush.”
“It’s funny how when we slow down, things become clearer faster.”
Psychedelics Today: Ido Cohen – Re-Turn to Wholeness: Jung and Integration
Psychedelics Today: PT271 – Jeremy Narby, Ph.D. – Anthropology, Ayahuasca, and Plant Teachers
Psychedelics Today: Katherine MacLean – Imagining Interesting Future
Psychedelics Today: PT305 – Emma Farrell – Plant Spirits, Entities, and Remembering Lost Traditions
 Dr. Ido Cohen, Psy.D, serves individuals, couples, and groups in San Francisco. As part of his practice, Ido works with a diverse range of challenges – childhood trauma, inner critic, relational issues, as well as integration and preparation sessions with individuals and groups. His doctoral dissertation was a 6-year study of the integration process of Ayahuasca ceremonies, while applying Jungian psychology to better understand how to support individuals in their process of change and transformation. He is also the founder of The Integration Circle and facilitates workshops on the different dimensions of integration and the intersection of mental health, spiritual health, and the entheogenic experience. Ido is passionate in supporting individuals to create longterm, sustainable change leading to vibrant, authentic, expressive, and love-filled lives.
Dr. Ido Cohen, Psy.D, serves individuals, couples, and groups in San Francisco. As part of his practice, Ido works with a diverse range of challenges – childhood trauma, inner critic, relational issues, as well as integration and preparation sessions with individuals and groups. His doctoral dissertation was a 6-year study of the integration process of Ayahuasca ceremonies, while applying Jungian psychology to better understand how to support individuals in their process of change and transformation. He is also the founder of The Integration Circle and facilitates workshops on the different dimensions of integration and the intersection of mental health, spiritual health, and the entheogenic experience. Ido is passionate in supporting individuals to create longterm, sustainable change leading to vibrant, authentic, expressive, and love-filled lives.
Socials: Instagram / The Integration Circle Instagram



In this episode of the podcast, Joe interviews Kathryn L. Tucker, JD: Special Counsel at Emerge Law Group, where she Co-Chairs the Psychedelic Practice Group.
Tucker has had a 35-year career in advocacy and protecting rights of terminally ill patients, serving as lead counsel in three landmark federal cases around constitutional rights and dying. Most recently, she was part of the team responsible for enacting Oregon’s groundbreaking Measure 109.
She discusses the mechanics of how access to psychedelic medicine works under the Right to Try act; how she feels about decriminalization vs. legalization and how it all relates to what she’s seen in the field of death and dying; what she’s excited about in Oregon; and how measures in Colorado could take things even further.
While synthetic psilocybin is the only “investigational drug” offered under Right to Try, naturally-derived psilocybin and MDMA could be an option sooner than we think – but based on the DEA’s behavior so far, that will only happen if more people join the fight, as it’s been over a year with no answer on how the DEA would be enabling psilocybin access to patients under the Right to Try act. To help push this along, Tucker welcomes donations, but more importantly, she invites activists everywhere to “shine the bright light of public scrutiny” on the insulting inaction of perhaps the government’s most ineffective agency. There’s a clear path here where everyone wins, so please, call your state’s elected officials and demand that they actually do their job.
“Part of what’s been so frustrating, of course, is when we satisfied ourselves as attorneys, that the state and federal right to try laws did in fact apply to psilocybin and that it should be accessible for therapeutic use with patients with advanced illness; when we approached the DEA to inquire how it would enable that access, that inquiry was in January of last year, 2021, so we’re now more than a year later and the DEA is still obstructing access.”
“To absolutely prohibit access, when state and federal law are intended to allow access; that is impermissible. …These dying patients could have immediate, substantial, and sustained relief from debilitating anxiety and depression. That’s what all the studies show, and I’ll say those words again because they’re the words that really caught my attention: immediate, substantial, and sustained relief. And why anyone would obstruct access to that kind of relief for a dying patient is impossible to comprehend.”
“I would just as soon not need to return to court, although I think our merits arguments are incredibly strong. I’d much rather see the DEA just adopt an attitude of: ‘Everyone can win here. Our interest in diversion protection can be addressed, the patient’s need for relief can be permitted and everyone can declare victory and go home.’”
Emergelawgroup.com: Kathryn Tucker Article archive
Thenowaksociety.org: Right to Try Psilocybin Advocacy Fund (where to donate)
The Right to Try act
Lucid.news: Terminally Ill Patients Fight for Access to Psilocybin Under Federal “Right to Try” Act
Northstar.guide (the Northstar Pledge)
Hereandnowstudios.com: We Will Call it PALA
 Kathryn L. Tucker, JD is Special Counsel at Emerge Law Group, where she Co-Chairs the Psychedelic Practice Group. Tucker is a founding member of the Psychedelic Bar Association and serves as Liaison to the Psychedelic Lawyering Task Force within the American Bar Association. Across her 30 year career, Tucker’s work has focused on advocacy to protect and expand the rights of the terminally ill. She served as Executive Director of the End of Life Liberty Project (ELLP), which she founded during her tenure as Executive Director of the Disability Rights Legal Center (DRLC), the nation’s oldest disability rights advocacy organization. Tucker served two decades as Director of Advocacy and Legal Affairs for Compassion & Choices. Prior to that, she practiced law with Perkins Coie. Professor Tucker has held faculty appointments at Loyola/Los Angeles, the University of Washington, Seattle University and Lewis & Clark, Schools of Law, teaching in the area of law, medicine and ethics at the end of life. Tucker served as lead counsel representing patients and physicians in two landmark federal cases decided by the United States Supreme Court, Washington v. Glucksberg and Vacco v. Quill, asserting that mentally competent terminally ill patients have a constitutional right to choose aid in dying. These cases are widely acknowledged to have prompted nationwide attention to improving care of the dying, and to have established a federal constitutional right to aggressive pain management. Tucker played a key role in successfully defending the Oregon Death with Dignity Act from attack by the United States Department of Justice, resulting in the landmark decision of the United States Supreme Court, Oregon v. Gonzales, representing the patient plaintiffs. Tucker was part of the team that succeeded in enacting the nation’s first state law permitting psilocybin therapy (Oregon Measure 109, 2020). She serves as lead counsel representing a palliative care physician and an oncology clinic in the first effort to apply Right to Try laws to psilocybin therapy, AIMS et al v DEA.
Kathryn L. Tucker, JD is Special Counsel at Emerge Law Group, where she Co-Chairs the Psychedelic Practice Group. Tucker is a founding member of the Psychedelic Bar Association and serves as Liaison to the Psychedelic Lawyering Task Force within the American Bar Association. Across her 30 year career, Tucker’s work has focused on advocacy to protect and expand the rights of the terminally ill. She served as Executive Director of the End of Life Liberty Project (ELLP), which she founded during her tenure as Executive Director of the Disability Rights Legal Center (DRLC), the nation’s oldest disability rights advocacy organization. Tucker served two decades as Director of Advocacy and Legal Affairs for Compassion & Choices. Prior to that, she practiced law with Perkins Coie. Professor Tucker has held faculty appointments at Loyola/Los Angeles, the University of Washington, Seattle University and Lewis & Clark, Schools of Law, teaching in the area of law, medicine and ethics at the end of life. Tucker served as lead counsel representing patients and physicians in two landmark federal cases decided by the United States Supreme Court, Washington v. Glucksberg and Vacco v. Quill, asserting that mentally competent terminally ill patients have a constitutional right to choose aid in dying. These cases are widely acknowledged to have prompted nationwide attention to improving care of the dying, and to have established a federal constitutional right to aggressive pain management. Tucker played a key role in successfully defending the Oregon Death with Dignity Act from attack by the United States Department of Justice, resulting in the landmark decision of the United States Supreme Court, Oregon v. Gonzales, representing the patient plaintiffs. Tucker was part of the team that succeeded in enacting the nation’s first state law permitting psilocybin therapy (Oregon Measure 109, 2020). She serves as lead counsel representing a palliative care physician and an oncology clinic in the first effort to apply Right to Try laws to psilocybin therapy, AIMS et al v DEA.



Health Canada’s recent SAP revision brings a new opportunity for patients and a clear responsibility for prescribers.
Health Canada’s recent decision to include psychedelic medicines in its Special Access Program (SAP) was met with a lot of fanfare. The SAP amendment brings good news for certain patients – specifically, treatment-resistant patients suffering from serious mental health conditions that impact individuals, families, and communities.
The new federal amendment has the potential to fill a critical gap for patients in need, including those suffering from depression, PTSD, and end-of-life anxiety. Many who suffer from mental health conditions don’t respond fully to current treatments, so there is a significant unmet need for safer and more effective therapies. The change to Health Canada’s SAP now allows physicians, clinics and hospitals to apply for previously restricted drugs for medical use, providing a new option for the patients who need it most.
I applaud the federal government for responding to the grave situation of the patients who aren’t responding to otherwise adequate treatment – and for recognizing the encouraging clinical data around psychedelic-assisted therapy. This SAP revision represents one small but important step on the road to greater access to psychedelic medicine.
Like most opportunities, this one comes with considerable responsibility. Failure to act responsibly could cause harm to individuals and to this evolving area of medicine. However, I believe that the community of experts in psychedelic medicine are ready and willing to support the practitioners who will be administering these therapies to patients.

Health Canada’s SAP revision adds certain psychedelics, including MDMA and psilocybin, to the list of restricted substances that practitioners can request to treat patients in specific situations. Decisions will be made on a case-by-case basis, and will be reserved for serious treatment-resistant or life-threatening conditions, in instances where other therapies have failed, or are unsuitable or not available in Canada.
The recent amendment reverses regulatory changes made almost a decade ago that prohibited access to restricted drugs (including psychedelics). Historically, practitioners in Canada have been able to apply for unlicensed medications only through Health Canada’s Section 56 exemption – a fairly long and restrictive process. The SAP revision is expected to provide a much quicker review and more rapid access for approved patients.
Obviously, the SAP amendment will not bring broad access to psychedelic medicine in Canada, but ideally will help treatment-resistant patients, and serves as a clear signal that the government is acknowledging the potential of psychedelic medicine as a legitimate treatment option.
To me, the government’s decision to include psychedelics in Canada’s SAP is a key acknowledgement that mental health conditions are being placed on the same footing as physical conditions, and frankly, that’s a shift that’s long overdue. Anyone working in mental health can see that treatment-resistant mental illness is indeed a serious or life-threatening condition, analogous to cancer that hasn’t responded to conventional treatment. But mental health disorders aren’t always viewed with that sense of urgency.
I’ve dedicated a good part of my medical career to raising awareness and advocating for changes in the treatment of mental health issues. I spent more than 30 years as a medical officer and psychiatrist in the Canadian Armed Forces, deploying twice and leading mental health programs in Afghanistan. I served as mental health advisor to the Canadian Forces surgeon general, and led initiatives with Canada and NATO as we explored innovative solutions in mental health. Achieving change in attitudes toward mental health and treatment innovation requires considerable effort and persistence.

We’ve seen modest improvement in mental health care over the years. However, I firmly believe we need to do better in this arena. Far superior advances have been made in the treatment of cancer, heart disease, and many other conditions that take an enormous toll on society and represent a significant medical and economic burden.
Yet in the field of mental health, so many patients continue to suffer without adequate or effective treatment. We must review the data while being mindful that each file or data point represents a person who is struggling. We must work to develop medicines with better results, realizing that mental health disorders affect not only patients, but their families and loved ones, their careers and communities.
During my time as the Chief of Psychiatry, I have experienced firsthand the enormous impact that trauma can have on soldiers and veterans. From mass graves in Rwanda to the battlefields of Kandahar, it’s difficult to see people who are putting their lives on the line to protect their country return home to treatments that will only work for half of them.
So the onus is on us to look for better solutions, to refuse to be satisfied with the status quo and to embrace ALL positive steps forward. In Canada, the inclusion of psychedelics in the SAP is one of those steps. That’s progress worth celebrating.
A growing body of evidence continues to demonstrate that psychedelic-assisted psychotherapies are emerging as a successful treatment option in many indications, from treatment-resistant depression to smoking and alcohol addiction to PTSD, anxiety, and OCD.
In the area of smoking cessation, Dr. Matthew Johnson and his team at Johns Hopkins are planning new studies to build on his team’s ongoing research, including the first government-funded clinical study in 50 years evaluating a psychedelic for therapeutic use. The team’s earlier study reported that 80% of participants who received psychedelic-assisted therapy remained abstinent from smoking at 6 months and 67% remained abstinent at 12 months. Those encouraging results show strong efficacy, and demonstrate clear progress.
We see positive data in other indications as well, including PTSD. MAPS is currently sponsoring MAPP2, the second of two Phase 3 trials studying MDMA-assisted therapy for PTSD. In the first Phase 3 study, 88% of participants with severe PTSD experienced a clinically-significant reduction in PTSD diagnostic scores two months after their third session of MDMA-assisted therapy, compared to 60% of placebo participants. Additionally, 67% of participants in the MDMA group (compared to 32% of participants in the placebo group) no longer met the criteria for PTSD remission two months after the sessions.
When governmental and regulatory agencies endorse the positive early results of new, transformative treatments, we can celebrate this success. And when organizations dedicate funding for continued research in our field, we applaud those decisions. We can use every bit of incremental progress as adrenaline to keep gathering evidence, and to use that evidence as our guide as we expand treatment options and promote best practices in administering them.
As Canada implements its recent change, the responsibility lies with clinicians and regulatory bodies to be very deliberate and safe in the way we use the SAP program. We must ensure that patient selection is based on science, and principles such as informed consent are followed.
I encourage doctors and patients considering these new treatment modalities to review the available research and have open, honest conversations with one another to determine if psychedelic-assisted psychotherapy is right for them. These are far from being first-line treatments and we must continue to turn to approved evidence-based treatments first.
Here’s the government’s process for requesting drugs through the SAP:
To administer psychedelic-assisted therapy under Health Canada’s SAP, healthcare professionals must fill out an application, which will be reviewed on a case-by-case basis.
The SAP considers a “healthcare professional” someone who:
Practitioners who receive approval can then request products from manufacturers that meet governmental requirements.
A few examples of questions asked in the application:
“What specifically about this drug makes it the best choice for your patient(s)?”
“Specify all treatments tried and/or failed…”
A request to provide references/evidence:
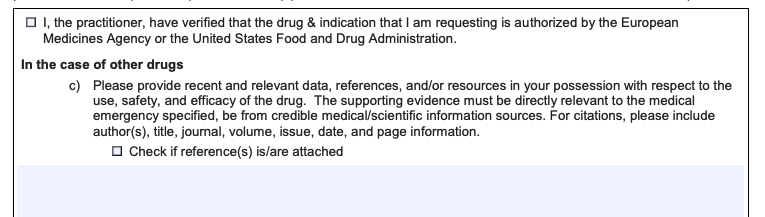
A question for a request for a repeat patient:
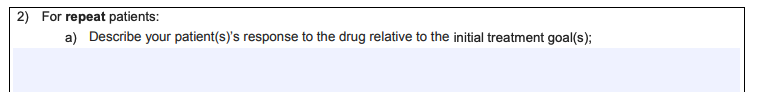
The final section:
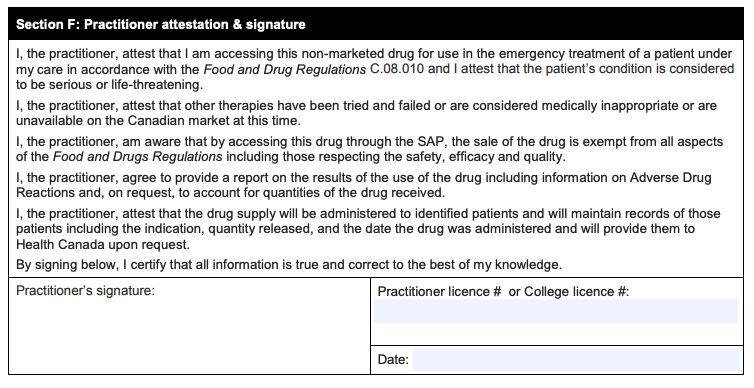
How progressive or cautious will Health Canada be in reviewing and approving requests? That remains to be seen. But as a physician, my advice is clear: The practitioners who seek permission to use these medicines should ensure that they have the necessary training, competence, and confidence to provide these treatments safely and successfully.
The innovators in our field are scientists, doctors, and advisors offering extensive experience with psychedelic compounds, as well as mental health and addiction disorders. We must step up and support physicians who want to prescribe these treatments, but who might not have experience implementing psychedelic-assisted psychotherapy. We can provide evidence-based research, education on proper protocols, and access to experienced psychedelic integration specialists to answer questions every step of the way.
My message is simple: Let’s do this right. Let’s do this safely.

The SAP should not be considered an alternative to integrating psychedelic-assisted therapy into existing medical practices. Rather, it provides help for those who qualify for use in exceptional circumstances under the SAP guidelines. It’s a step forward, but it’s not a solution.
Psilocybin and MDMA-based therapies are successful with specific indications and patient profiles. We need to continue gathering data to demonstrate safety and efficacy through clinical trials targeting specific indications. That’s the path to obtain regulatory approval of psychedelics with therapy protocols. Psychedelics must undergo the same rigor as any other medication vying for approval from regulatory bodies. We need to continue the work that will lead to an environment of safe, regulated access to psychedelic therapy in a medical setting. That takes patience, but will pay off in the long run.
Ultimately, the millions of patients afflicted with serious mental illness will benefit most when they have access to more advanced, more effective therapies than those on the market today. We truly see success when medical communities view psychedelic medicine as an accepted and adopted form of treatment within our existing healthcare infrastructure.
In this episode of Vital Psychedelic Conversations, Kyle interviews Dr. Devon Christie: Senior Lead of Psychedelic Programs with Numinus Wellness, clinical instructor, counselor, and Co-Investigator and study therapist for a Canadian MAPS-sponsored trial investigating MDMA-assisted therapy for PTSD.
Christie talks about the importance of biomedical ethics and the unique considerations of psychedelic-assisted therapy: how psychedelics enhance the vulnerability and suggestibility in a well-established power dynamic, and how being aware of your power and biases is of the utmost importance towards not influencing your patient’s experience. They discuss just how much that experience is affected by every detail of preparation, and how it’s a very thin line between scaring someone off, setting impossible expectations, or even giving away too much of the experience (and with limitless possibilities, is that even possible?).
And she talks about the complications of touch and establishing (and honoring) informed consent; how true mindfulness can cultivate a greater capacity for self-regulation; how to handle situations where the client wants to know if a memory is real or not; the idea of psychedelics as a placebo; and many other complicated therapeutic concepts like harm of neglect, undue influence, making pleasure a virtue, cultivating agency, combating physician burnout, and the expectation effect.
“We don’t really know, but there may be aspects of psychedelics and their impacts that may make them ultimately like super placebos.”
“From my training as a relational somatic therapist, it’s actually not about the facts or details of what happened that matter. In fact, we can resolve trauma without even recollection of facts or details because we’re working with how it shows up in the body and how it’s showing up emotionally. …We can assist that process through working with what’s actually emergent in the felt experience and not needing to stay adherent to the narrative around it.”
“I think the yardstick on how far we’re going with this psychedelic work is that, either personally in our own journeys or even in the folks we’re supporting, we’re getting to a place where we don’t need the psychedelics – where the psychedelics have given us a reference, they’ve opened up new vistas of possibility, they’ve helped us to approach our lives differently, such that we are now cultivating the quality of presence and the quality of investigation and curiosity and flexibility and all those things that psychedelics can bring us – in our ordinary lives. …We’ve got these tools and they can help us learn and they can help us connect, and then hopefully we can come full circle and we can drop the tools and just be able to live meaningful lives that are sustaining for ourselves and for each other.”
Healing Moments in Psychotherapy, Edited by Daniel J. Siegel and Marion F. Solomon
PT297 – Laura Mae Northrup, LMFT – Radical Healership in a Profit-Driven World
 Dr. Devon Christie is a medical doctor and registered counselor with a focused practice in chronic pain and trauma. She is trained to deliver both MDMA-assisted therapy for PTSD and ketamine-assisted psychotherapy, and she serves as Senior Lead of Psychedelic Programs with Numinus Wellness. Devon is also a certified Mindfulness Based Stress Reduction teacher, Functional Medicine practitioner, and clinical instructor with UBC Family Medicine. She is currently Co-Investigator and study therapist for a Canadian MAPS-sponsored trial investigating MDMA-assisted therapy for PTSD, and co-investigator on a pilot study investigating MDMA-assisted therapy for fibromyalgia.
Dr. Devon Christie is a medical doctor and registered counselor with a focused practice in chronic pain and trauma. She is trained to deliver both MDMA-assisted therapy for PTSD and ketamine-assisted psychotherapy, and she serves as Senior Lead of Psychedelic Programs with Numinus Wellness. Devon is also a certified Mindfulness Based Stress Reduction teacher, Functional Medicine practitioner, and clinical instructor with UBC Family Medicine. She is currently Co-Investigator and study therapist for a Canadian MAPS-sponsored trial investigating MDMA-assisted therapy for PTSD, and co-investigator on a pilot study investigating MDMA-assisted therapy for fibromyalgia.
Devon is passionate about educating future psychedelic therapists on trauma-informed, relational somatic skills. She also teaches for the California Institute of Integral Studies (CIIS) Certificate Program in Psychedelic Therapy and Research, the Integrative Psychiatry Institute Certificate Program in Psychedelic Assisted Therapy, and the ONCA Foundation Psychedelic Therapy program.
Socials: Instagram / Facebook
Numinus: Instagram / Facebook / Twitter



In this episode of the podcast, Joe interviews Adam Bramlage: Founder and CEO of Flow State Micro, a functional mushroom company and microdosing educational platform.
Bramlage talks about his journey to psychedelics and discovery of microdosing, and how he worries that the troubling issues he saw in the legal cannabis industry are already finding their way into the psychedelic space. He discusses what he experienced when he started microdosing; how he connected with James Fadiman; how he defines microdosing; the concepts of neurogenesis and a gut-brain axis; how more and more professional athletes are using psychedelics to heal brain injuries as well as optimize performance (and how leagues may handle this going forward); concerns over chronic microdosing; and why the goal is always to microdose less over time.
While we expected to hear about the benefits of microdosing, their conversation also goes deep into its history and our ancestral connection to psychedelics (particularly psilocybin), touching on Hernán Cortés; R. Gordan Wasson banking for the vatican; Christianity, Jesus, and mushrooms; repeated examples of control through the erasure of history; Tim Leary; Al Hubbard; MKUltra; the Tarahumara Indians’ peyote-influenced ultra-running; cave paintings; Whitey Bulger, and more.
Bramlage is a speaker on May 27th’s Microdosing Summit (along with Joe), and just released a new “Microdosing Movement Masterclass” in collaboration with the San Francisco Psychedelic Society, which focuses on our ancestral connection to psychedelics and the potential evolutionary use of microdosing. Use code psychedelicstoday at checkout for 10% off!
“I’m a single dad to two kids, and both of those kids, at periods of time in their life, were raised on a cannabis farm. And what I’ll tell you is this: when you normalize these plants and these tools and it’s just like a flower or a squash that my kid sees farmed like the farmer next to me, my kids want nothing to do with cannabis. It is so uncool. It’s the last thing they want to be around. I don’t have any worries about my son or daughter smoking pot. And why? Because we normalized it. And if you look at Portugal and what they’ve done with drugs and the success they’ve had with decrim legalization, supporting substance abuse issues with therapists and programs; this is the future. This is the answer.”
“We have an ancestral and evolutionary connection to these plants and it’s only in the last couple hundred years that they’ve been made illegal and bastardized. …We’re putting five or six year old kids on Adderall (which is methamphetamine), but we’re pointing fingers at a parent who gives their kid 10 milligrams of a mushroom.”
“Psychedelics have an afterglow, or a 48-hour effect, so you don’t need to microdose seven days a week. You can take it on a Monday, take Tuesday off, and you’re still getting benefits. So what I see over time with microdosing is the more people use it, the less they need it. This isn’t a Western medical model of: you’re going to take microdoses five days a week because it regulates your blood pressure and your heart condition. It’s not like that. This is more like: the more people are microdosing over time, the less they need it. …When I’m coaching people or working with clients, the goal is to eventually not microdose.”
Psychedelicsocietysf.org: The Microdosing Movement Masterclass
Microdosing Summit: May 27th (International Microdosing Day)
Doubleblindmag.com: “How to Microdose” class
The Broken Spears: The Aztec Account of the Conquest of Mexico, by Miguel Leon-Portilla
The Sacred Mushroom and The Cross, by John M. Allegro
The Immortality Key: The Secret History of the Religion with No Name, by Brian C. Muraresku
Trippingly.net: Al Hubbard: The Original Captain Trips
Ultrarunninghistory.com: The Tarahumara Ultrarunners
Secret Drugs of Buddhism: Psychedelic Sacraments and the Origins of the Vajrayana, by Mike Crowley
Gnosticwarrior.com: Whitey Bulger: Crime Boss Said CIA Gave Him LSD in Mind Control Experiment
 Adam Bramlage is Founder/CEO of Flow State Micro, a functional mushroom company and microdosing educational platform focusing on harm reduction and best practices. Bramlage works one-on-one with clients to optimize their microdosing experience. He’s helped hundreds of people, from professional athletes to people suffering from addiction and depression, achieve incredible results through microdosing. Bramlage works closely with psychedelic researcher, pioneer and father of modern microdosing, Dr. James Fadiman. In collaboration with Doubleblind Magazine, Bramlage launched his 14 episode online course “How to Microdose,” which was recently featured in Forbes Magazine as one of the masterclasses of psychedelics, and received an award from Gear Report for Top Ten Wellness Products of 2021. In collaboration with the SF Psychedelic Society, he has recently released his online Microdosing Movement Masterclass, looking at our ancestral and potential evolutionary use of microdosing. He is co-founder of the Microdosing Support Network, the first free online monthly microdosing support group. Prior to his work with mushrooms, he spent more than a decade in the Prop 215 and Prop 64 California cannabis space as a farmer, distributor, and manufacturer. He hopes psychedelics does NOT go the same route as legal cannabis.
Adam Bramlage is Founder/CEO of Flow State Micro, a functional mushroom company and microdosing educational platform focusing on harm reduction and best practices. Bramlage works one-on-one with clients to optimize their microdosing experience. He’s helped hundreds of people, from professional athletes to people suffering from addiction and depression, achieve incredible results through microdosing. Bramlage works closely with psychedelic researcher, pioneer and father of modern microdosing, Dr. James Fadiman. In collaboration with Doubleblind Magazine, Bramlage launched his 14 episode online course “How to Microdose,” which was recently featured in Forbes Magazine as one of the masterclasses of psychedelics, and received an award from Gear Report for Top Ten Wellness Products of 2021. In collaboration with the SF Psychedelic Society, he has recently released his online Microdosing Movement Masterclass, looking at our ancestral and potential evolutionary use of microdosing. He is co-founder of the Microdosing Support Network, the first free online monthly microdosing support group. Prior to his work with mushrooms, he spent more than a decade in the Prop 215 and Prop 64 California cannabis space as a farmer, distributor, and manufacturer. He hopes psychedelics does NOT go the same route as legal cannabis.



In this episode of Vital Psychedelic Conversations, Kyle interviews clinical psychologist, author, and researcher, Dr. Adele Lafrance.
Lafrance developed Emotion-Focused Family Therapy, which focuses on the role of the family in psychedelic work. Realizing that the healing process disrupts systems and that dealing with a loved one who is going through a massive shift can be quite challenging for their loved ones, the idea behind EFFT is teaching family and significant others emotion-processing and behavioral support skills, how to make therapeutic apologies, how to recognize defensiveness and not react in a knee-jerk way, and how to find problematic caregiving problems where families accommodate for mental health issues (and therefore perpetuate them). While not typical for adults to involve significant others or family in therapeutic processes, she has found that if done correctly, it can be extremely helpful.
She talks about anger: how we struggle with expressions of anger, the idea of healthy anger, and the ways psychedelics can help us move from rejecting anger to assertion. And she discusses the Hoffman Process; emotion coaching; the power of validation; similarities between EFFT and IFS; rolling with resistance; tips to incorporate family into therapy more; the concept of a shame hangover and checking in on “tomorrow you”; and that even with all the preparation in the world, there’s no way to adequately prepare someone for the vast array of possibilities within (and after) a psychedelic experience.
In addition to being one of the faculty of Vital (reminder that applications close on March 27th), Dr. Lafrance has a 4-Part, CE-approved EFFT Core Clinician Training course that begins April 4th. Click here for details.
“As a culture, we really, really struggle with healthy expressions of anger, both in delivering them and in receiving them, so we end up having these unconscious contracts with our loved ones where there’s this unspoken rule that we don’t …speak up for ourselves when we feel like things aren’t going okay, and both parties can be ‘okay’ with that. And one thing that psychedelics does …is that they help us connect to our healthy assertion, as a byproduct of the cultivation of self-love.”
“The paradox of rolling with resistance is that that’s exactly the most efficient route to releasing resistance.”
“There’s actually no way to adequately prepare for what might come. And so I’ve incorporated that – this idea [that] there could be major shifts that are highly disruptive, you might reconnect to old memories that you completely lost connection to that are not pleasant and that will shake your world, or, you can have an experience of self-love that helps clarify your path forward in your career, and anything in between. …We don’t know what can happen. We don’t know. It can be a smooth re-entry, or it can feel like your life blows up, and you need to be prepared for that. What I do know, though, is that it is way more likely that anything that happens will be in the service of creating a more aligned life for you. That, I do feel comfortable saying.”
“Integrity is about doing your ultimate best, being supported, asking for help, and then when you fall down, you pick yourself back up, you learn from your mistakes, and then you teach others.”
DrAdeleLafrance.com: The Love Project
Clinicaltrials.gov: Psilocybin as a Treatment for Anorexia Nervosa: A Pilot Study
Chacruna.net: Ayahuasca and the Power of Forgiveness
Chacruna.net: Love and Psychedelic Psychotherapy: Bridging the Divide
DrAdeleLafrance.com: Events (4-Part, CE-approved EFFT Core Clinician Training/equivalent 2-Day Training with Dr. Adele Lafrance begins April 4th)
Sciencedirect.com: MDMA-assisted therapy significantly reduces eating disorder symptoms in a randomized placebo-controlled trial of adults with severe PTSD
Psychedelics Today: Rapid Depression Remission and the “Therapeutic Bends” with Ketamine-Assisted Psychotherapy
 Dr. Adele Lafrance is a clinical psychologist, research scientist, author, and co-developer of emotion-focused treatment modalities, including Emotion-Focused Family Therapy. A frequent keynote speaker at professional conferences, Adele has published extensively in the field of emotion and health, including a clinical manual on EFFT published by the American Psychological Association. She is passionate about helping parents to support their kids in a way that is informed by the latest developments in neuroscience. The knowledge and tips in her book, What to Say to Kids When Nothing Seems to Work is an effort to do just that. With colleagues, she also makes a wealth of caregiving resources available at no cost at Mental Health Foundations.
Dr. Adele Lafrance is a clinical psychologist, research scientist, author, and co-developer of emotion-focused treatment modalities, including Emotion-Focused Family Therapy. A frequent keynote speaker at professional conferences, Adele has published extensively in the field of emotion and health, including a clinical manual on EFFT published by the American Psychological Association. She is passionate about helping parents to support their kids in a way that is informed by the latest developments in neuroscience. The knowledge and tips in her book, What to Say to Kids When Nothing Seems to Work is an effort to do just that. With colleagues, she also makes a wealth of caregiving resources available at no cost at Mental Health Foundations.
Adele is also leader in the research and practice of psychedelic medicine, with a focus on ayahuasca, MDMA, psilocybin and ketamine. Currently, she is the clinical investigator and strategy lead for the MAPS-sponsored MDMA-assisted psychotherapy study for eating disorders and a collaborator/clinical support on the Imperial College study for psilocybin and anorexia nervosa. She is a founding member of the Love Project.



In last week’s blog, Ed Prideaux told us everything we know (and don’t) about Hallucinogen Persisting Perception Disorder (HPPD), visual snow syndrome, and flashbacks. In part 2, he addresses ways to deal with the distress of having HPPD and ways to reduce the risk of developing it in the first place.
The real “problem” with HPPD is distress: anxiety, depression, isolation, panic, and the unhelpful coping mechanisms people can develop to overcome these (alcoholism and drug dependency are sadly common among HPPD patients). Remember, this distress is what technically defines HPPD.
Many people live with significant visual changes and do not find them distressing – rather, they may be sources of enjoyment, “free trips,” artistic inspiration, or purposefully leaned into as part of spiritual or occult practice. The world looking different doesn’t necessarily mean you have a problem.
If you’re currently experiencing HPPD, though, overcoming the distress should probably be your first priority. Speaking crudely, once the distress is overcome, the visuals can more or less “take care of themselves.” With less distress, there is less fixation. With less fixation, there is less noticing. With less noticing, the visuals are less noticeable. They may rapidly normalize, filter in the background, and can disappear unexpectedly with time.

Medication and clinical help:
Many in the HPPD community have found relief in the use (especially in the short-term) of medications including Lamotrigine and Klonopin. They can bring visuals and anxiety way down, though some report their symptoms getting worse. They can always bring side effects, too, so some caution is advised.
Do not be surprised, either, if clinicians have not heard of HPPD. It is little-known and poorly-understood. It may be useful to refer your clinician to the Information Guide included on the Perception Restoration Foundation’s website.
Healthy lifestyle changes:
Many HPPD patients report the decline and resolution of their symptoms – or otherwise acceptance and returning to “normal” life after avoiding further drug-taking, exercising regularly, cutting out processed foods, or trying specific elimination diets.
Noting Triggers:
Pay attention to your triggers and act accordingly. Visuals and other HPPD symptoms can surface in response to:
You should also pay special attention to how your condition manifests beyond visuals, in particular, if you are experiencing Depersonalization/Derealization Disorder. More than visuals, it’s often the case that people’s distress comes from DP/DR, and a rich body of literature and therapeutic approaches have been explored for this condition.

Community: You can seek community from others, such as groups on Facebook, or the forums at HPPDOnline.com, r/HPPD, or r/visualsnow. However, tread cautiously around spending too much time on these forums. They can be extremely negative, and cause people to spiral and fixate on their perceptual changes.
Mindfulness meditation: The stress reduction and relaxation effects of meditation are well-established; many report breaking the cycle of visual fixation through learning to hone their attention.
Cognitive techniques: Cognitive Behavioral Therapy (CBT) and Acceptance and Commitment Therapy (ACT) may be useful for accepting and reframing perceptual changes. Challenging the internal beliefs triggered by HPPD could reduce both distress and the visuals – in particular, the beliefs that patients are “brain damaged,” “weird,” “isolated,” or a “casualty.”
Psychedelic integration: Introspection, journaling, and (if you can find and afford it) specialist, psychedelic-informed counseling can be helpful. In particular, you may benefit from exploring the particular details and events of what may have caused HPPD to originally materialize.
Somatic approaches: Certain somatic/bodily therapies have proven helpful for people with Visual Snow Syndrome. This includes the use of acupuncture, muscle relaxation techniques, neck massage, and specific dietary interventions.
Reframing: It may be helpful to learn that many people are not troubled by their perceptual changes. Again, they can be just a “thing” – how one sees now – that’s different, and not necessarily bad. Other people actively enjoy their perceptual changes or view them in a spiritual way, such as glimpsing auras, having broadened the possibility of the mind, or in seeing the intrinsic shakiness of ordinary experience.
Without a deep, embodied grounding for your reframing, though, it can be hazardous. Make sure the frame is not just “in your head,” but truly held across your entire mind and body in a felt way. Don’t gaslight yourself into enjoying your perceptual changes if they are actually disturbing you.

There is reason to suspect that the immediate period after a trip – say, one-to-five days – is important. This is because the brain is still neuroplastic and affected by psychedelics for up to a week (or longer) after the trip. And HPPD may be understood as a problem of “resetting” one’s brain back into its ordinary perceptual categories after the shock of a psychedelic experience.
If you want to avoid HPPD, what matters is ensuring that your perception re-transitions to its prior sober state safely. In this one-to-five day period, it may be advised, then, to:
Have you optimized your set and setting?
HPPD seems to be more likely after bad trips or challenging experiences – the likelihood of which strongly depends on how people organize their set and setting. In particular, stress and trauma going into a psychedelic experience may be a trigger for HPPD experiences, even at low dose (and microdose) levels.
Have you experienced some unusual visuals before?
HPPD patients may have had a higher-than-normal experience of certain visual oddities, which are rare parts of normal perception. In particular, phenomena like visual snow, halos, after-images, floaters, and colors in the dark may suggest an underlying tendency in perception that could be triggered by a psychedelic drug to be more intense.
Have you tested your drug? If so, what drug are you taking?
HPPD may be more likely with Novel Psychoactive Substances (NPSs) and Research Chemicals (RCs) with more unpredictable, less-researched, and possibly neurotoxic effects. Adulterants in street drugs may also have neurotoxic and other risky properties.
It seems that long-acting psychedelics like LSD are more likely to cause HPPD. While LSD may have certain advantages over other psychedelics subjective to each user, someone very conscious of developing HPPD (at least compared to other risks) may wish to avoid LSD in favor of a shorter-acting psychedelic.
How often are you tripping?
Taking lots of psychedelics frequently is likely to be correlated with a higher risk of developing HPPD. This can be explained in a number of ways:
For more, this article’s tips, advice, analysis (and more) is also featured in a more in-depth HPPD Information Guide, which can be freely downloaded from the Perception Restoration Foundation’s website, where a more direct guide for those struggling with HPPD is also hosted. Owing to the tentative nature of our HPPD knowledge base, the PRF invites any and all comments and criticisms for the Guide at info@perception.foundation, and any worthwhile amendments will be quickly published.
In this episode of the podcast, David interviews Chief of Staff, Head of Operations, and “Chief Cheerleader Officer” at Nue Life, Kabir Ali.
Ali speaks about the power of ketamine-assisted therapy and how his first ketamine treatment made him overcome 10 years of addiction and depression (and realize what caused it). He talks about addiction: his struggles, how people can have these relationships with anything, concerns over the addictive properties of ketamine, and the importance of having the right people in your corner – especially when using a substance to overcome another. And he talks about the lack of education in mental health he’s seen in his travels, how our current society seems to be driving us to escape, and how self-love (and the authenticity and freedom that comes from it) is one of the most overlooked and wonderful gifts of psychedelic-assisted therapy.
And he discusses Nue Life: how the clinicians he works with are magical people, the benefits he’s seen from integration work in group settings, the health coaching they’ve made a large part of their program, what he’s most excited about, and why he views Nue Life as a next-gen mental health company rather than a ketamine clinic.
“We’re certainly living in a space today where our environment is pushing us to escape. It doesn’t necessarily feel safe. There’s a lack of certainty in our social landscape over here today. And whenever I come by someone who is struggling with addiction, whether it’s someone that I am mentoring or personally coaching, it’s quite apparent that we cannot underestimate the value or the impact of our environment.”
“That self-compassion, that self-love: it’s one of the most, I think, overlooked gifts of these treatments.”
“The biggest gift, again, is that self-compassion, that self-care, that self-love. But the authenticity and the freedom that comes through these discoveries or through these experiences that we share with psychedelics; that’s one thing that I think we, at times, look over, which is: what is it that you are actually walking away with when you embark on a journey with plant medicines or with ketamine? And that’s just really the authenticity that you just touched upon right now, and that is that liberating feeling where we can actually go ahead and pursue and live the lives that we once had, or perhaps, lead a life that we never knew that we could lead.”
Lovediscovery.org: Dr. Carolina Pataky
 Kabir Ali is an advocate for accessible and innovative mental health care. As an operations executive in the wellness industry, his passion is to create collaborative teams that provide effective treatment at the highest standards of compliance. Kabir grew up in West Africa and Bombay and began his career as an actor and filmmaker in Bollywood. The pressures of the entertainment industry and the incarceration of a close family member ultimately led to struggles with addiction. While in treatment, he began working in healthcare communications, where he found satisfaction using his storytelling skills to help others heal. Today, Kabir serves as COO of Mind Body Medicine and My Ketamine Home and as Head of Operations for Nue Life, a recently-launched startup that provides at-home psychedelic therapy. In his spare time, Kabir studies the intersection of addiction and family systems and looks forward to developing additional programs that bring affordable mental health treatment to underserved communities.
Kabir Ali is an advocate for accessible and innovative mental health care. As an operations executive in the wellness industry, his passion is to create collaborative teams that provide effective treatment at the highest standards of compliance. Kabir grew up in West Africa and Bombay and began his career as an actor and filmmaker in Bollywood. The pressures of the entertainment industry and the incarceration of a close family member ultimately led to struggles with addiction. While in treatment, he began working in healthcare communications, where he found satisfaction using his storytelling skills to help others heal. Today, Kabir serves as COO of Mind Body Medicine and My Ketamine Home and as Head of Operations for Nue Life, a recently-launched startup that provides at-home psychedelic therapy. In his spare time, Kabir studies the intersection of addiction and family systems and looks forward to developing additional programs that bring affordable mental health treatment to underserved communities.
Nue Life socials: Instagram / Facebook / Twitter



In this episode of Vital Psychedelic Conversations, Kyle and David interview the author of No Bad Parts: Healing Trauma and Restoring Wholeness with the Internal Family Systems Model, and the creator of the IFS model itself: Dr. Richard C. Schwartz.
If you aren’t familiar with the Internal Family Systems model, this podcast serves as a great introduction, as Schwartz discusses how it came about and what it entails; how he views the Self; how IFS relates to the body; exiles, managers, and firefighters; the 8 Cs of self-leadership qualities; how to address the actions of one’s different parts; and how often people in psychedelic-assisted therapy sessions find themselves naturally thinking within the IFC framework. He believes that the different parts of the mind each have valuable qualities and resources, and psychedelics (and other non-ordinary states of consciousness) can help to re-harmonize the damaged parts, therefore allowing the Self to do its job as the inner healer.
He also talks about the importance of preparation and facilitators knowing their own parts; his psychedelic history and why he’s no longer afraid of death; what he strives for in integration work; the 5 Ps facilitators need; Sandra Watanabe’s concept of a “cast of characters”; soul retrieval; starling murmuration; and the Pixar movie, “Inside Out.”
“[Michael Mithoefer) kept track of how often, spontaneously, the subjects would start doing IFS without any coaching from the facilitators, and in the high-dose MDMA [studies], 80% would start working with parts spontaneously. And that felt very validating to me, like I had just stumbled onto a process that people naturally do once they access enough Self.”
“There are times where you just can’t convince these protective parts to let us get to an exile and heal it. And a psychedelic session can expedite that pretty easily, it seems.”
“For me, there is a big SELF, with all capitals, that’s kind of like the ocean, and then we’re a drop of that ocean – there’s a piece of that that’s in each of us that I’m calling the Self with a capital S. And when we take ketamine and we leave [our bodies], we’re actually going back into that ocean. And there’s a lot of bliss, at least for me. I mean, there [were] a few moments that weren’t so blissful, but much of it was just– I came back, and I say this and people find it hard to believe, but I have no fear of death now. I just know that it’s a transition into that ocean.”
“I think the psychedelic world has been conditioned by a kind of passivity approach to being present with people and just trusting their own process. And that can do a certain amount of good, but you’re also missing the opportunities [for] doing some really deep healing.”
IFS-institute.com: Richard C. Schwartz, Ph.D. – Bio and Appearances
SandraIngerman.com: Soul Retrieval
Psychedelics Today: Psychedelics and The Shadow: The Shadow Side of Psychedelia
Goodtherapy.org: Gestalt Therapy
Springer.com: Cast of characters work: Systemically exploring the naturally organized personality
Dau.edu: Debono’s Six Thinking Hats
Birdfact.com: Starling Murmuration: A Complete Guide
FoundationIFS.org: Make a donation
 Dr. Richard C. Schwartz began his career as a family therapist and an academic at the University of Illinois at Chicago. There, he discovered that family therapy alone did not achieve full symptom relief, and in asking patients why, he learned that they were plagued by what they called “parts.” These patients became his teachers as they described how their parts formed networks of inner relationship that resembled the families he had been working with. He also found that as they focused on, and thereby, separated from their parts, they would shift into a state characterized by qualities like curiosity, calm, confidence, and compassion. He called that inner essence the Self and was amazed to find it even in severely-diagnosed and traumatized patients. From these explorations, the Internal Family Systems (IFS) model was born in the early 1980s. IFS is now evidence-based and has become a widely-used form of psychotherapy, particularly with trauma. It provides a non-pathologizing, optimistic, and empowering perspective, and a practical and effective set of techniques for working with individuals, couples, families, and more recently, corporations and classrooms. In 2013, Schwartz left the Chicago area and now lives in Brookline, MA, where he is on the faculty of the Department of Psychiatry at Harvard Medical School.
Dr. Richard C. Schwartz began his career as a family therapist and an academic at the University of Illinois at Chicago. There, he discovered that family therapy alone did not achieve full symptom relief, and in asking patients why, he learned that they were plagued by what they called “parts.” These patients became his teachers as they described how their parts formed networks of inner relationship that resembled the families he had been working with. He also found that as they focused on, and thereby, separated from their parts, they would shift into a state characterized by qualities like curiosity, calm, confidence, and compassion. He called that inner essence the Self and was amazed to find it even in severely-diagnosed and traumatized patients. From these explorations, the Internal Family Systems (IFS) model was born in the early 1980s. IFS is now evidence-based and has become a widely-used form of psychotherapy, particularly with trauma. It provides a non-pathologizing, optimistic, and empowering perspective, and a practical and effective set of techniques for working with individuals, couples, families, and more recently, corporations and classrooms. In 2013, Schwartz left the Chicago area and now lives in Brookline, MA, where he is on the faculty of the Department of Psychiatry at Harvard Medical School.
Internal Family Systems socials: Instagram / Facebook / Twitter



Hallucinogen Persisting Perception Disorder, or HPPD, is among the more mysterious, debilitating, and under-researched possibilities of psychedelic drug-taking. As enthusiasm around psychedelics and their possible benefits continues to grow, it’s imperative that researchers, user populations, and clinicians look closely at HPPD and other possible hazards.
HPPD is little-known among clinicians, and many reporting these experiences have trouble finding informed help. Treatments – pharmacological, psychotherapeutic, and somatic – are out there, and by reports, have proven useful for some, but no controlled trials have been performed to gauge their true effectiveness.
In this article – intended as an exercise in harm reduction, raising awareness, and ensuring true informed consent before people ingest psychedelics – we’ll outline the current knowledge base around HPPD, including indications of the gaps and where future research may prove useful. This article’s tips, advice, and analysis (and more) is also featured in an in-depth HPPD Information Guide, which can be freely downloaded from the Perception Restoration Foundation’s website, where a more direct guide for those struggling with HPPD is also hosted.
Hallucinogen Persisting Perception Disorder is a DSM-5 listed condition in which people experience lasting, distressing changes to their perception after taking psychedelic drugs. There are two types: Type-1, in which people experience episodic (usually sudden) “flashbacks,” and Type-2 (the more commonly reported), in which people’s everyday perception is altered.
These perceptual changes may be married with shifts in cognition, mood, and somatic experience, and further research is required to understand how they relate. HPPD can last anywhere from weeks and months to several years – some people live with its perceptual changes for decades. In up to 50% of HPPD patients, the changes may spontaneously remit within five years.
The perceptual changes are wide-ranging, but most constellate around a stable set of experiences also reported in other conditions: Visual Snow Syndrome (VSS), migraine with aura, manic episodes, epilepsy, anxiety disorders, brain injuries, and also as experienceable features (under the right conditions) of normal, healthy perception.

This implies that HPPD likely sits on a continuum with other disorders and ordinary perception. Further research is required to understand HPPD’s role in this continuum, the possibly unique contribution of psychedelics in affecting symptoms, and the kinds of treatments people with HPPD would benefit from versus other disorders.
Other, non-perceptual symptoms are reported, too:
Note, to be diagnosed with HPPD, these changes must prompt distress – which they do, in many cases. They can disrupt people’s everyday function – relationships, work, operating heavy equipment, driving, navigating the day-to-day, and beyond – and cause anxiety, panic attacks, depression, and suicidal thoughts in high numbers of clinical patients. Many report a strong degree of isolation and loneliness, and the disorder is also strongly-correlated with dissociative experiences like Depersonalization/Derealization Disorder (DP/DR).
We don’t know. It seems that developing perceptual changes after taking psychedelics is not necessarily that uncommon; the distressing, intrusive kind that manifests in HPPD is likely a real but minority experience.
A 2011 survey of 2,455 users of psychedelics (via Erowid) found that up to three-fifths of psychedelic users reported lingering changes, 25% in ways that were seemingly permanent, and 4.2% in ways so distressing that they could prompt seeking clinical help. The latter is suggestive of diagnostic HPPD.

Practically every psychedelic, but some more than others: LSD, psilocybin, ayahuasca, 2-CB, ibogaine, etc., but also related (but not classically psychedelic) drugs like MDMA, cannabis, dextromethorphan (DXM), datura, ketamine, salvia, and diphenhydramine (DPH) have been implicated.
In anecdotal reports and the existing literature, it seems that LSD is the leading cause of perceptual changes compared to other kinds of drugs. Whether this is because LSD has been historically the most commonly-used psychedelic or there is something special to the LSD experience or its effect on neurophysiology is unclear. Short-acting psychedelics like DMT seem to be less implicated.
Some report that, after heavy use of classic psychedelics, their HPPD developed suddenly after the use of research chemicals like 25-i-nBOME, which is often mis-sold as LSD; HPPD is also reported in particular among users of synthetic cannabinoids. Cutting agents in street MDMA, including synthetic cathinones (“bath salts”), may make HPPD more likely.
Yes. SSRI antidepressants, antibiotics, antipsychotics, and nootropics have been described in self-reports as triggering very similar visual changes. There is also considerable overlap between HPPD/post-psychedelic perceptual changes and another drug-free condition known as Visual Snow Syndrome (VSS).
At the same time, compared to other drug classes, it seems that psychedelics (in particular, LSD) provide a higher risk factor for developing these perceptual changes. It may also be that HPPD patients report different kinds of visuals (perhaps more psychedelic ones), or more cognitive and emotional changes (as with psychedelics’ powerful psychoactive effects), compared to non-psychedelic groups.
It’s complicated. The “flashback” describes a particular kind of experience in which people feel they truly re-live a prior psychedelic state: something that is real and can happen, and is what people may experience in Type-1 HPPD. Most cases of Type-2 HPPD, though, will likely not be true examples of flashbacks in this way.
To give a brief overview, the idea that psychedelic drugs could cause lasting changes in perception was noted from as early as 1954 – 15 years before the notion of the “flashback” was ever coined. A number of authors in the first wave of psychedelic research from the 1950s to the early 1960s reported patients experiencing a wide range of complications after their drug experiences – including what sounds like standard HPPD – but also states that blur more into psychosis and the experience of complex pseudohallucinations. They noted that some patients were acutely re-living their trips.
These observations continued once psychedelics became popular drugs of adult use in the mid-to-late 1960s. This was reported in popular media from, at latest, 1966.
The “flashback” label was coined by author Mardi J. Horowitz in 1969, and used for many years afterwards, including by Dr. Henry Abraham, who first developed the psychiatric diagnosis of HPPD. Perhaps contrary to what we’d expect, authors in the “flashback” literature were at pains to emphasize the complexity, variation, and need for further research in explaining the phenomenon, as well as noting that many (some surveys suggested the majority) did not find their experiences distressing.
Unfortunately, the idea of the flashback was later sensationalized by journalists and prohibition activists, who tied the idea to certain marked untruths: that the drug can be “stored” in the spine or fat cells, make people legally insane, or otherwise cause major brain damage.
The flashback idea also had some conceptual problems, which is perhaps to be expected from the first attempts at describing a new phenomenon. With some critical exceptions, authors were bound by a consensus that post-psychedelic visuals and flashbacks were re-experiences of the visuals glimpsed in the psychedelic state – as if the drug had not properly worn off, perhaps as a matter of lasting changes to neurological function. The notion that HPPD is a “re-experiencing” has also become one of the core criteria of the current DSM-5 diagnosis.
As noted earlier, though, identical perceptual phenomena can be experienced both through non-psychedelic drug classes, and as part of experiences in which drugs played no necessary role: other kinds of neuropsychological conditions, or otherwise as a feature of normal perception.
In contemporary literature, some authors have noted that many patients experience visual effects that never manifested in their trips – though this isn’t the case for everyone. Those who are “reliving” their trips may be described plausibly as experiencing flashbacks.
The idea of the flashback is also not unique to psychedelics – in particular, it’s used as a descriptor for experiences of post-traumatic stress disorder (PTSD), in which people can feel “flung back” to the original trauma in quasi-visionary states. This implies that the psychedelic “flashback” may not be a distinct phenomenon for some (or most) cases: rather, that it’s an example of a psychedelic drug-induced traumatic flashback, where the real issue is trauma (not drugs per se).

Since authors first noticed that psychedelics can cause lingering changes in perception, a variety of different hypotheses have been pursued to explain what’s going on. The HPPD experience will likely involve a complex, multi-factor origin that varies from patient to patient.
Could psychedelic experiences alter neurophysiological function?
HPPD’s leading neurophysiological hypothesis, introduced by Dr. Henry Abraham, relates the condition to a “disinhibition” of the visual cortex. Drugs like LSD decrease, or “disinhibit” the filters of the brain’s visual cortex, so visual noise that would otherwise be filtered out may remain in the field of vision. HPPD occurs when these filters do not return to their pre-drug state. This may make HPPD akin to a form of “visual tinnitus” (and tinnitus is also experienced as a symptom).
This disinhibition is linked to reductions in alpha waves in the brain. A neuroimaging study by Abraham (2001) suggested that alpha wave frequency increases with HPPD patients versus controls. The role of an objective alteration to visual perception was lent support by 1982 and 1988 studies executed by Abraham, in which he found both non-HPPD LSD users and HPPD patients had decreased ability to discriminate color differences and light sensitivity during dark adaptation, with HPPD patients reporting further decreased ability.
There could be a role for neuroplasticity, or neurons’ ability to change and reform in response to experience. This may be explained in the context of a “Bayesian Brain” model, similar to the REBUS and entropic brain hypotheses introduced by UCSF’s Robin Carhart-Harris: by shaking the “snowglobe” of our nervous system’s categories of perception through a psychedelic experience (or psychoactive changes altogether), it could be that those categories do not settle as before. A neuroplasticity model may explain why, in some cases, further psychedelic experimentation can reduce or eliminate HPPD presentation. It may underlie also why teenagers are especially vulnerable, as they have more plastic, developing brains.
LSD’s long duration may explain why the drug is so associated with HPPD – that is, with more hours of seeing abnormal visual changes, the brain is more likely to reprogram itself than with shorter-acting drugs. Smokeable DMT, for instance, isn’t particularly-associated with perceptual changes, while longer-acting ayahuasca is.
Synaptogenesis may also be involved. As described by Samuel Štancl, “Psychedelics induce strong synaptogenesis, or the creation of new synapses, resulting in high synaptic density. EEG scans show less inhibitory activity in the visual cortex both in people on psychedelics and in people with HPPD.” This means that electrical currents are being enhanced in the visual cortex by increased synaptic connection. This also underwrites why pruning excessive synapses through pharmacological treatments like lithium – or even exercise – may be useful.
What about psychological factors?
A 2018 paper by Halpern and Passie suggested that challenging drug experiences, including intense reactions of panic, dysphoria, anxiety and trauma, may be associated with a higher likelihood of developing HPPD. This is more likely for psychedelic use in uncontrolled settings.
Recall, HPPD often co-arises with Depersonalization/Derealization, a dissociative reaction in which people feel disconnected from their bodies and immediate environments. This is suggestive of anxiety and trauma. Drug-free anxiety and depersonalization are independently-associated with similar, if not identical, perceptual changes. Somatic cognitive changes, including head pressure and brain fog, are also associated with anxiety. Challenging and traumatic drug experiences may therefore induce elevations of anxiety, which has its own uncharted pathway towards many changes, including perception.
In the historical flashback literature, there was tentative evidence that visual phenomena could be experienced as matters of attention, hypnotization, and placebo suggestion. The role of trait absorption – or a person’s tendency to become occupied by mental imagery and internal experience, including daydreaming, fantasy and hypnagogia – has also been discussed by authors as a possible personality determinant of HPPD likelihood.
What’s more, there are case reports of people altogether resolving their distress and visuals through targeted psychotherapies without pharmaceuticals: in particular, Cognitive Behavioral Therapy (CBT) to target the destructive internal beliefs people formed around their condition (“I am brain damaged,” “I’m a weirdo,” “I’m a freak,” etc.), including in combination with relaxation techniques. The sense of isolation may also be addressed through the therapist leaning into their own capacity for abnormal visual phenomena, and experiencing them with the patient – something that resolved one person’s HPPD.
Psychedelic researcher Stanislav Grof explained and resolved his patients’ cases of HPPD through psychodynamic therapies. He interpreted HPPD as a problem of the psychedelic surfacing unconscious material that needed to be re-integrated through additional encounter experiences, including with psychedelics and breathwork.
Could HPPD patients simply be noticing more stuff that previously filtered into the background?
Yes, at least for some patients. Phenomena like visual snow, after-images, tinnitus, and floaters are not necessarily uncommon, even among “normal” people. As a possibly overlapping mechanism with anxiety and fixation, it may be that some people with HPPD are noticing perceptual features that had previously been filtered into the ignorable background of their experience. Halpern and Passie found that HPPD patients were possibly more likely to have experienced visual oddities before they took drugs.
This led Krebs and Johansen to recommend re-attributing some HPPD experiences to Somatic Symptom Disorder, whereby people fixate and ruminate on normal somatic experiences and perceptions.
This is unlikely to be exhaustive, because many HPPD patients report florid and extreme visual changes that plausibly could not have been ignored before; it will also have limited applicability to those whose visuals are distinctly psychedelic and are experiencing Type-1 HPPD. It’s possible, too, that histories of such visual experiences imply a vulnerability that has been activated or catalyzed by drug experiences.
Part 2 of this article, focusing on harm reduction, will be posted shortly!
This article’s tips, advice, analysis (and more) is also featured in a more in-depth HPPD Information Guide, which can be freely downloaded from the Perception Restoration Foundation’s website, where a more direct guide for those struggling with HPPD is also hosted. Owing to the tentative nature of our HPPD knowledge base, the PRF invites any and all comments and criticisms for the Guide at info@perception.foundation, and any worthwhile amendments will be quickly published.
In this episode of the podcast, Joe interviews Ed Prideaux: UK-based writer and journalist working to raise awareness around Hallucinogen Persisting Perception Disorder (HPPD) in affiliation with the Perception Restoration Foundation.
While HPPD is known in the psychedelic community (Kyle has unfortunately had experience with it), it’s not talked about or researched enough, and often considered by many as fake or a trauma reactivation. Prideaux likes to call HPPD “post-drug perceptual changes,” and talks all about it: how it came about in his life and how it affects him; what visual snow syndrome and other common HPPD visuals look like; big names in the field and current research; neurodiversity and looking at things from a “critical psychiatry” lens; how he thinks HPPD relates to anxiety and distress from depersonalization effects and isolation (did you know that visual changes are reported in people with generalized anxiety disorders?); and how so much of the lack of knowledge and progress around HPPD is a direct result of the drug war.
Is there a higher chance of HPPD happening when the experience happens in youth? Are there dormancy effects? Is cannabis a larger trigger than people think? Is the biggest trigger being overwhelmed by a larger-than-expected dose? Is LSD the most commonly reported culprit due to how long the trip is? Is one unintentionally training their brain to get used to a trip during these long experiences? Could entering into more non-ordinary states of consciousness actually be the solution?
The Perception Restoration Foundation is working on a study in Macquarie University in Australia looking at neuroimaging of people with HPPD, they just released an HPPD information guide in collaboration with MAPS, and they are working to finalize and release a documentary called “HPPD: Stuck in an Altered World” that features someone at least Joe and this show notes writer are huge fans of: Andrew Callaghan of Channel 5 News (previously of “All Gas No Breaks”). We will have a companion piece about HPPD from Prideaux in the blog this week as well.
“I remember lots of experiences where I’d be in my living room with my parents (who had no idea what I was going through) and I’d look at my Dad, I’d look away, and a complete afterimage of his silhouette would linger in the air for several seconds. Walls would morph, I’d see faint geometric patterns on the floor and on surfaces at school; surfaces, walls, carpets – they would melt and move waxly, like I was in a kind of semi-psychedelic state. There’d be times when I’d glance over at the carpet and there would be faint mandalas and kaleidoscopes on it. …The worst effect of these visual changes; it wasn’t so much anxiety about what I’d done, it was just the sheer sense of isolation, as if I was stuck in my own essentially mini broken perceptual world that I was just too freaked out to tell any of my friends or family about.”
“I don’t want to be a savior guy here, but these severe HPPD cases have, for the longest time, been essentially left voiceless. And I hope that this film will be the voice and mouthpiece for them.”
“I think part of the HPPD problem is our culture’s entire warped relationship with drugs, in particular, in creating the conditions for the sense of isolation and self-shame that can come with HPPD. …With drugs, it seems to be that there’s limited room for empathy. It’s just like, ‘Yeah, you’re a druggie and this is what you did to yourself. You fried your brain.’ The brain-frying thing; it’s a huge source of self-stigma for people with HPPD. I definitely experienced it myself in the first year after I developed the condition, like, ‘Yeah, I’m a basket case. I’m an acid casualty.’ And I think that all of these really needlessly self-shaming, incredibly negative and unpleasant narratives people tell themselves are allowed to fester in a culture where we can’t have open conversations about the risks and benefits of drugs.”
“In the current environment we’re in with the psychedelic renaissance, we’re in a delicate pivotal time for psychedelics. And obviously, this is psychologizing for other people and projection is playing a role here, but I think people can feel self-conscious about coming out and saying, ‘Hey, yeah, I have actually been having some difficulty from my trips,’ because they don’t want to spoil the fun. They don’t want to derail the train.”
Edprideaux.journoportfolio.com
YouTube: “HPPD: Stuck In A Distorted World” trailer
Psychreg.org: Changing Your Brain State Through the Ganzfeld Effect
HPPDonline.com: Perception Foundation’s HPPD study at Macquarie University
Madnessradio.net (Will Hall’s podcast)
The Myth of Mental Illness: Foundations of a Theory of Personal Conduct, by Thomas S. Szasz, M.D.
Psychedelicreview.com: Psychedelics and Perception Part 1: Visual Effects
 Ed Prideaux is a UK-based writer and journalist who’s written about psychedelics for the BBC, VICE, The Independent, and Unherd, and other topics for The Guardian, The Financial Times, The Spectator, and The Quietus. Ed is working to advocate and raise awareness around Hallucinogen Persisting Perception Disorder (HPPD) in affiliation with the Perception Restoration Foundation, a new 501 (c) (3) nonprofit that has secured the launch of HPPD’s first breakout studies in decades.
Ed Prideaux is a UK-based writer and journalist who’s written about psychedelics for the BBC, VICE, The Independent, and Unherd, and other topics for The Guardian, The Financial Times, The Spectator, and The Quietus. Ed is working to advocate and raise awareness around Hallucinogen Persisting Perception Disorder (HPPD) in affiliation with the Perception Restoration Foundation, a new 501 (c) (3) nonprofit that has secured the launch of HPPD’s first breakout studies in decades.
.



In this episode of Vital Psychedelic Conversations, Kyle interviews Michael Sapiro, PsyD: clinical psychologist, writer, meditation researcher, integrative coach, former Buddhist monk, Vital teacher, and now 3-time podcast guest.
They begin with what he feels is the most vital conversation we should be having now, then he discusses the idea of bringing psychedelics to prisons; his mental time travel work with The Institute for Love and Time (TILT); building an ecosystem where those with means pay full price to enable those with less money a discount; rebuilding trust in the medical community; and the difference between a diploma and real-world experience and proper training.
And he talks about the mystical experience, working with clients, and education: how so much more training is necessary than people realize, and how so much of the true education is learning how to vocalize an internal experience (and then integrating the positive aspects into everyday life). He talks about the complicated dynamics involved in what many see as a fantasy career; how he knows when to intervene; how he views “doing your own work”; whether or not the work can be gentle or joyous; the idea of joking during a session; his work with combat veterans and the intensity of 5-MeO-DMT; mainstreaming mysticism; and trusting that the universe has our backs.
“We want people to have real, internal experiences that they’re aware of and they can vocalize, and that is the actual education; not just the knowledge I’m giving them about what this drug does to the brain or how you identify something. It’s really: What is alive in you, how do you identify what’s alive in you, how do you use it in real time, and then how do you navigate those circumstances and change and grow? That’s the real learning process.”
“The mystical experience is a present moment experience where the universe unfolds in front, within, and around you, and then we integrate that into our human self. So Mike gets this amazing introduction to the universe through an experience and then it comes in and becomes insight and knowledge, and then hopefully practical application. So that’s where I think, in the end, we actually transform; is when that knowledge becomes integrated into the fabric of our own being [and] into our personality, and now Mike and the universe are more melded.”
“Zen is serious until you learn the universe is playful, and then you get to be kind of playful with it.”
“My hope is that all of us touch on the unconditional love that’s here for us, within us. And once you touch that, you can’t not offer it. You can’t not take care of other things. …This work gives us access to what’s already fundamentally true, and helps us bridge that with everything else.”
Loveandtime.org (TILT: The Institute for Love and Time)
Springer.com: Mental Time Travel? A Neurocognitive Model of Event Simulation
Start with Why: How Great Leaders Inspire Everyone to Take Action, by Simon Sinek
 Michael Sapiro, PsyD, is a clinical psychologist, writer, meditation researcher, and former Buddhist monk. He is on faculty at Esalen Institute, is a Fellow at the Institute of Noetic Sciences, and is completing a study on time travel, hope, and love with Dr. Julia Mossbridge of The Institute for Love and Time. Dr. Sapiro teaches nationally on the art and science of transformation, expanded human capabilities, and futuremaking. He is the integrative psychologist at the Boise Ketamine Clinic where he offers Ketamine-Assisted Psychotherapy (KAP and KAT) sessions, and is an integrative coach with VETS, helping former Navy Seals and other special operations team members recover from combat exposure with psychedelic-assisted therapy. He hosts a syndicated radio program called Radio Awakened out of KRBX. His work is dedicated to personal awakening for the sake of collective and planetary transformation. He can be found at Michaelsapiro.com.
Michael Sapiro, PsyD, is a clinical psychologist, writer, meditation researcher, and former Buddhist monk. He is on faculty at Esalen Institute, is a Fellow at the Institute of Noetic Sciences, and is completing a study on time travel, hope, and love with Dr. Julia Mossbridge of The Institute for Love and Time. Dr. Sapiro teaches nationally on the art and science of transformation, expanded human capabilities, and futuremaking. He is the integrative psychologist at the Boise Ketamine Clinic where he offers Ketamine-Assisted Psychotherapy (KAP and KAT) sessions, and is an integrative coach with VETS, helping former Navy Seals and other special operations team members recover from combat exposure with psychedelic-assisted therapy. He hosts a syndicated radio program called Radio Awakened out of KRBX. His work is dedicated to personal awakening for the sake of collective and planetary transformation. He can be found at Michaelsapiro.com.



In this episode of the podcast, Kyle interviews Laura Mae Northrup, LMFT: author, educator, somatic psychotherapist, and host of Inside Eyes, a podcast focusing on the use of psychedelics for healing sexual trauma.
Northrup is the author of the just-released Radical Healership: How to Build a Values-Driven Healing Practice in a Profit-Driven World, which, although not focused on psychedelic work specifically, was largely written on or inspired by psychedelics, and is beneficial for people entering the field as psychedelic practitioners (she calls it “a self-help book for healers”). She talks about the book and ways to make a sustainable path towards a healthy practice, with the most important factors being to build in time for joy and inspiration, and to continuously do your own work.
She discusses what “doing your own work” really means; what people struggle with when entering the field; the idea of ”action movie therapy”; the ways gained power, unconscious motivations, or issues you haven’t worked on can influence the ways you work with others; why preparation is maybe more important than integration; capitalism and why practitioners shouldn’t feel bad about charging money for their services; the importance of trauma training; the need for community and developing relationships with colleagues; and why, while society usually feels differently, you don’t actually have to be perfect to become a healing practitioner.
If you’re interested in Radical Healership, we have a discount code for you thanks to North Atlantic Books! Go here and use code psychedelicstoday for 30% off and free shipping!
“What you’re doing, especially if you’re working in a psychological or spiritual realm, is that you’re using your own being as your instrument. And so, just like somebody who is a surgeon that is using a surgical knife; you would want that person to be cleaning that surgical knife and replacing it when it’s dull and really tending to this surgical knife. This isn’t the same as just trying to cut up a tomato for dinner and it’s okay if the knife gets a little dull over the years. You want to make sure your instrument is well cared for, and that is you. It’s your being.”
“We’re so obsessed with the pinnacle moment or the peak experience that we don’t value appropriately all of the more mundane experiences that actually allow that peak experience to happen safely. Absolutely, the people I see doing the most profound healing work for themselves [and] getting a lot out of psychedelic medicine; they did a lot of prep. We talk a lot about integration, I think, in the community, but we don’t talk as much about preparation, and I actually think integration flows a lot more easily if you’ve done a lot of preparation.”
“There’s kind of this fantasy healing practitioners can get into where they’re like, ‘I’m not going to charge anything’ or ‘I’m going to charge really little.’ And I would say one individual person driving themselves into lifelong debt and not charging enough money is not actually changing the system. I think it’s masochistic. I think a lot of healing practitioners do it, and to all the healing practitioners listening right now that struggle with this, I want to speak to you and I want to say: I want you to be a okay, because we fucking need you so that you can actually help people heal, and when you’re driving yourself into the ground and stressed out and you can barely support yourself, you’re not taking care of yourself enough to support other people. So please charge enough to be okay.”
“Finding our way through capitalism involves connecting ourselves to a deep, deep, deep sense of love.”
Psychedelics Today: Laura Northrup – Healing Sexual Trauma with Psychedelics and Entheogens
Psychedelics Today: Psychedelics and The Shadow: The Shadow Side of Psychedelia
Psychedelics Today: Horizons: Grounds for Collective Effervescence, by By Jessica (Jaz) Cadoch, MA (Northrup’s Horizons speech is discussed)
 Laura Mae Northrup, LMFT is an author, educator, somatic psychotherapist, and podcaster. Her book Radical Healership (Feb 2022) is a spiritually-informed and anticapitalist guide for healing practitioners who seek to build a values-driven healing practice. She is the host and creator of the podcast Inside Eyes, an audio series about people using entheogens and psychedelics to heal from sexual trauma. Her work focuses on defining sexual violence through a spiritual and politicized lens, mentoring healing practitioners in creating a meaningful path, and supporting the spiritual integrity of our collective humanity. You can learn more about her work here: www.lauramaenorthrup.com.
Laura Mae Northrup, LMFT is an author, educator, somatic psychotherapist, and podcaster. Her book Radical Healership (Feb 2022) is a spiritually-informed and anticapitalist guide for healing practitioners who seek to build a values-driven healing practice. She is the host and creator of the podcast Inside Eyes, an audio series about people using entheogens and psychedelics to heal from sexual trauma. Her work focuses on defining sexual violence through a spiritual and politicized lens, mentoring healing practitioners in creating a meaningful path, and supporting the spiritual integrity of our collective humanity. You can learn more about her work here: www.lauramaenorthrup.com.
Instagram / Twitter / Facebook



Prolonged negative body image will often lead to depression and anxiety, and unfortunately for many people, can lead to body dysmorphia or an eating disorder. Could psychedelics help reframe one’s relationship with their body?
Psychedelics offer promise for those who struggle with eating disorders – 9% of the world’s population according to the National Association of Anorexia Nervosa and Associated Disorders.
These conditions primarily impact women, and now more of them are coming forward to share how psychedelics are helping them leave a constant cycle of dissatisfaction, body dysmorphia, and the accompanying anxiety, depression, and stress. They explain how the use of psychedelics helped them develop a new relationship with their eating disorders and improve their self-image.
While large-scale studies are (currently) scarce, the anecdotal evidence of these shifts is powerful.
“The first time I sat with a hero’s dose of magic mushrooms, I realized I could put my eating disorder down and never carry it again,” shares Francesca Rose, who is now an eating disorder recovery advocate. “It finally clicked: my eating disorder was not part of me. It wasn’t even mine. It all made sense. I was free from my eating disorder. I no longer needed to control food or my body to feel safe or worthy.” Having her life changed through the use of psychedelics and being on the recovery path for 13 years, this psychedelic-assisted shift is part of what led her to add her current work; supporting other women with eating disorders along their healing journeys.
For many women, talking about their insecurities is still seen as a taboo, weakness, or shameful. Yet finding a supportive space to speak of one’s challenges, plus engaging in embodied experiences – including psychedelic sessions – can offer a gateway to healing. Rose’s work also includes leading embodiment practices via yoga and conscious dance. By helping women speak of their struggles and reconnect to their bodies, she aims to break these stigmas.
Adding in the intentional and safe use of psychedelics can allow women to reconnect with their bodies and cultivate a gentler relationship with themselves. Rose says, “An eating disorder is unconsciously employed as an attempt to feel protected in the world and to even give a sense of meaning and identity. The internal world is fractured and the eating disorder is a way to try to stitch things together, even if it’s an unsustainable method. When we are journeying with psychedelics and engaging in post-journey integration, people can find they rely less on the eating disorder because there is a general sense of ease in the world and more internal wholeness. We can get in touch with our essence, and connect with our inherent worth, belonging, dignity and divinity. Psychedelics can help us embody pride and self-acceptance. We can connect to love, and feel our capacity to give and receive love.”

To have a better understanding of these conditions, we need to first comprehend body image. For most women, it’s not as simple as liking or disliking their own bodies. Body image is complex, and can include a combination of our feelings, beliefs, and perceptions of how our body looks to us and others, the understanding of what it can do, and its estimated size.
Body image issues can start as early as 5 years old. Changes to our physiques kicked off by puberty can deepen our dissatisfaction. Culture also exerts a huge influence on the way we view ourselves. The way society sees gender, the color of skin and hair, and countless other things can also impact the way a person thinks and feels about their physical appearance.
Body dysmorphia is a psychological disorder characterized by an excessive concern for the body, causing the person to overvalue small imperfections or even imagine imperfections. This creates a negative body image and lowers self-esteem. It can drive possible eating disorders and problems in social, professional, and personal lives. Both men and women may experience body dysmorphia and eating disorders, though women are three times more likely to have their lives affected by it.
In the United States, approximately 30 million people suffer from some type of eating disorder. Of these 30 million, 70% do not have the assistance of a specialized professional. As a consequence, anorexia nervosa, one of the most common eating disorders, has a 5.9% mortality rate – one of the highest rates within mental health conditions.
Eating disorders are notoriously challenging to treat relative to other mental health disorders. Traditional treatments, such as Cognitive Behavioral Therapy (CBT), have a remission rate of about 45%, a relapse rate of about 30% within one year, and can be hard to follow. Now, some experts and researchers are considering psychedelic therapy as an alternative, and are analyzing the potential benefits of this treatment.
“Eating disorders typically develop as maladaptive coping mechanisms when internal resourcing is overwhelmed by what’s happening in a person’s life,” says Lauren Taus, a California-based therapist who offers ketamine-assisted sessions. Taus and other therapists who contributed their perspectives for this piece say that psychedelic therapy can alleviate the symptoms that are normally associated with these conditions, such as depression and anxiety, in ways that traditional therapy fails to achieve. As Dr. Adele Lafrance points out in this article for EdCatalogue, psychedelic therapy has “the potential to alleviate symptoms that relate to serotonergic signaling and cognitive inflexibility, and the induction of desirable brain states that might accelerate therapeutic processes.”
Taus shared an example of her own work with psychedelics as an alternative treatment that helped her with many of her challenges, including her eating disorder: “My experience with empathogens has invited me to see how much conflict was warring inside of me. I saw all the pain of my personal history, and all that was beyond my control in my family system. Fundamentally, these psychedelics invited me to directly process what was beneath the surface. I accessed great grief, rage, and fear while opening to deep levels of love and compassion for myself and everyone else. I understood my parents and the choices they made, so I could forgive them. I also sourced the willingness, desire, and strength to fight for myself – and my life.”
So what is it about psychedelics specifically that can facilitate profound breakthroughs like Taus’? For starters, they can positively impact the Default Mode Network (DMN), which handles communication between brain regions. This region appears to be hyperactive in some mental health conditions, including depression, anxiety, and OCD. And certain hallmarks of eating disorders, such as the poor cognitive flexibility seen in many anorexia nervosa patients, may also be related to an overactive DMN. Studies such as “Rethinking Therapeutic Strategies for Anorexia Nervosa: Insights From Psychedelic Medicine and Animal Models” indicate that psychedelics lower the activity in this area, and, by doing so, allow us to create new thought patterns, giving us a fresh perspective on life, the world, and ourselves.
Another way that psychedelic psychotherapy can be effective is by helping a person understand the true source of their feelings of dissatisfaction. A 2013 analysis of why eating disorder therapy fails reveals that a patient’s resistance stems from the disorder’s “ego-syntonic” nature. Ego-syntonic means that the ego’s demands and aspirations drive many of the disorder’s behaviors, feelings, and values. Psychedelic substances can offer a temporary dissolution of the ego, allowing the possibility of transformation, healing, and change of certain behaviors, thought patterns, or addictions.
Taus explains that “Psychedelic assisted psychotherapy supports embodied change where traditional psychotherapy often stays in the realm of cognition and intellect. A person, for example, may come to understand with depth and clarity their patterns in therapy, but still struggle to shift them.” For example, a woman might know that purging is a harmful behavior that leads to feelings of shame. “She may even know exactly why and when it all started, but still she may not be able to stop. Psychoactive substances can create experiential shifts that more efficiently translate into internally-led and sustained behavioral change. The job of the therapist is to provide a safe container for the exploration and a good relational context for a person to make sense of the experience and to anchor in the good that comes from it.”
It’s important to highlight that the use of psychedelic substances on their own does not work as a magic bullet and treatments must be done alongside psychotherapy and/or other healing modalities such as journaling and yoga. A holistic approach seems to be the most effective path to long-term healing for women with eating disorders and body dysmorphia.
Ketamine, ayahuasca, MDMA, and psilocybin are the four psychedelics that have been the focus of the majority of the latest research for the potential treatment of eating disorders. Let’s take a look at how each one could help with eating disorders:
Ketamine:
Ketamine is a non-classical psychedelic that can alter consciousness for a short period of time. This synthetic compound’s antidepressant qualities have been researched for treating severe depression, PTSD, and OCD.
Ketamine can be administered through IV, injected, taken orally, or it can be insufflated (blown into a body cavity, such as the nasal passages). The dose is titrated according to weight, with the understanding that everyone metabolizes the medicine differently. Ketamine is known for its dissociative effects, such as feeling like things are moving in slow motion or that you are separated from reality, with objects looking different and other characteristics that can be seen in this study.
“With regards to ketamine, the dissociative experience can translate into more joy in embodied experience. Ketamine-Assisted Psychotherapy (KAP) creates a break from the ordinary mind and a loosening of the belief systems that eating disorders are so rigidly held by. From a scientific perspective, psychedelics interrupt the default mode network, which governs self-image, memories, beliefs, and patterns.” says Taus. “The drug essentially creates an opportunity to reorganize the brain into a system that is more supportive for good living. Ketamine also results in increased neuroplasticity, which creates a golden hour opportunity for potent therapy work with a client 24-48 hours after a KAP experience.”

A few studies include: Treatment of compulsive behaviour in eating disorders with intermittent ketamine infusions, Ketamine and Activity-Based Anorexia, and the ongoing work of Dr. Adele LaFrance with Emotion-Focused Family Therapy.
Ayahuasca:
Ayahuasca is a fermented herbal drink that contains dimethyltryptamine (DMT), one of the most potent psychedelic drugs known for its role in shamanic or religious ceremonies. The brew has been utilized as a sacred ritual by various South American Indigenous tribes for at least 1000 years. Journeyers frequently claim mystical and transcendent visions that lead to self-discovery.
The first ever study of ayahuasca’s potential to help people heal from eating disorders was published in 2017, co-led by Dr. Adele Lafrance and Dr. Kenneth Tupper. The majority of the people in the study said that ayahuasca helped to reduce their eating disorder symptoms and showed them the root cause of the disorder. Regarding the purging effects of the brew, participants found it easy to differentiate between an eating disorder purge, and the purge of an ayahuasca experience.
The ayahuasca experience has the ability to favorably affect behavior, stimulating self-reflection and increased awareness. Studies suggest that drinking it can aid in the treatment of anxiety, addictions, and depression, as well as eating disorders by also shifting body perceptions.

One study is: An exploratory study of experiences with conventional eating disorder treatment and ceremonial ayahuasca for the healing of eating disorders.
MDMA:
MDMA, another laboratory-created compound, has a physiological effect that alters people’s behavior such as openness. MDMA boosts serotonin levels while also upping oxytocin, dopamine, and other chemical mediators, resulting in feelings of empathy, trust, and compassion. The substance also has an effect on the way people process trauma and emotions for a period of several hours.
In clinical settings, MDMA is taken orally in capsules. The patient first takes a full dose (75-125 mg) and has the option to add a second dose about 2 hours into the session. An MDMA session will typically last between 6 to 8 hours.
MDMA causes an increase in prefrontal cortex activity, which is important for information processing, and a slowing in the amygdala, the part of the brain that is key in processing memories and emotions associated with fear. The key therapeutic benefit of MDMA is its capacity to excite the brain, allowing it to create and store new memories. Patients become more emotionally flexible and capable of exploring challenging memories during psychotherapy sessions, which often leads to long-term changes in how they react to emotional changes.

A few studies include: The potential use of MDMA assisted psychotherapy in the treatment of eating disorders comorbid with PTSD, A Multi-Site Study of MDMA-Assisted Psychotherapy for Eating Disorders (MED1).
Psilocybin:
Psilocybin is a substance generated by more than 100 different mushroom species around the world. Psilocybin is said to have the best safety profile of all psychedelic substances. The fungi could be useful in the treatment of eating disorders by targeting the brain’s serotonin imbalance and therapeutically shifting the person away from symptom-focused treatment. This could establish changes in self-worth and self-compassion.
Aside from that, the efficacy of psilocybin therapy in the treatment of OCD shows how it could be useful in the treatment of eating disorders, as obsessive thoughts and compulsive and obsessive actions are also common hallmarks of eating disorders.

One study is: Effects of Psilocybin in Anorexia Nervosa.
Psychedelics can help women see their eating disorder as a coping mechanism and not as part of their identity. Once they embody this insight, they can also slowly start to replace bad habits with healthier and kinder new habits. They can rewrite the inner narrative of lies and self-limiting beliefs about their bodies.
Once more, there is a need to emphasize the importance of integration, relationships, and a holistic approach alongside other therapeutic methods and modalities. Change comes with time, effort, and consistency, especially when deconditioning behaviors that have been a big part of our lives for many years.
When asked about how long it takes for those changes to fully take place, Rose points out that “Eating disorders and addiction are transformational experiences that hold enriching value. Indeed, the word, ‘transformation’ means change or conversion. When thinking about recovery, it is not about stopping or restricting a behavior but rather allowing it to change and transform, taking us along for the ride so that our beliefs, feelings, thoughts, behavior, and action take a new form. Grounded, sustainable change does not happen overnight.”
“For me, recovery is about inner personal and spiritual growth, and incremental daily, positive changes. My experience with eating disorders and addiction has led me to believe that they offer lessons and advantages, transforming me into more of who I truly am: alive, free, appreciative, and connected.”
Although more research is still needed to better understand the safety and efficacy of psychedelic medicines and therapy in the treatment of eating disorders, the promising results we’re seeing show that this is a worthy goal to pursue. Stories such as Rose’s and Taus’ are just two among many other women who have experienced transformational change thanks to these compounds.
“With the support of therapy, community, spirituality, and relationships, I no longer judge my body, or effort to dominate her,” says Taus. “My experiences with plant medicines have supported me in understanding my body as a perfect part of nature, and in much the same way that I don’t complain about the shape of a leaf or a wave, I accept – even appreciate – the parts of me I’ve historically struggled with.”
“The power of psychedelic-assisted therapy is in its experiential quality,” she says. “When knowing meets feeling and understanding, we can galvanize the courage and strength needed to shapeshift our lives and reconstruct ourselves.”
In this episode of Vital Psychedelic Conversations, David interviews Andrew Tatarsky, Ph.D.; author and developer of Integrative Harm Reduction Psychotherapy, and Juliana Mulligan; writer and head of Inner Vision Ibogaine, which supports people in their preparation for and integration of ibogaine treatment. Both are involved with our Vital program, and both are part of The Center for Optimal Living in NYC (CFOL); Tatarsky as the Founder and Director, and Mulligan as the Psychedelic Program Coordinator.
Mulligan tells her story of overcoming opioid dependence through an almost deadly ibogaine treatment, and how later, she began to see two major issues quickly becoming a problem: the continued labeling of psychedelic interventions as “miracle cures,” and the alarming lack of knowledge so many people seemed to have about preparation and integration. Tatarsky discusses his realization that traditional 12-step or abstinence-only programs were contributing to what he calls “treatment trauma,” and how breaking the rules in how he treated people led to a newfound interest in harm reduction and the creation of the CFOL.
They talk about reframing addiction, the ways society divides us by accepted behaviors, how being taught to doubt ourselves as children creates trauma, the idea of the “disease narrative” and self-demonization, how research studies support the idea of the quick fix, and harm reduction as a pathway to a better self.
The CFOL is currently running an 8-week virtual training series with a focus on intersectionality and social justice called “Working with Psychedelics to Treat Substance Use Issues,” featuring names like Gabor Maté, Laura Mae Northrup, Courtney Watson, and Dr. Carl Hart. Mulligan developed the curriculum by asking her favorite people in the psychedelic space what they were most passionate about. Check out the event page here.
“The harm reduction framework is about not imposing barriers, expectations, our values [and] our agendas on the people that we’re trying to be helpful to. It’s about radical acceptance and respect and empowerment, and therefore we can truly meet people where they are as unique humans in unique social and relational environments and create a safe space to support people in discovering their truth and their goals and what approach to positive change makes sense to them. So it’s non-ideological, it’s non-prescriptive, and I think it really is a very powerful way of engaging folks. And it works!” -Andrew
“I had to go through homelessness and getting beaten up and going to jail and all of this, but the most traumatizing thing for me was being told repeatedly that I had a disease for life that had no cure and I had to admit that I was powerless and say that I was an addict for the rest of my life, and if I stopped going to these meetings, then I would end up in a jail, institution, or I would die.” -Juliana
“In the psychedelic world in general, we need to get away from this kind of ‘miracle’ language or even ‘10 years of therapy in one night.’ That kind of thing, I think, is playing into the notions that we’ve been taught in capitalism that you can buy your way into getting what you want or there’s some kind of magical overnight fix for things. There’s not.” -Juliana
“We’re losing hundreds of thousands of people a year from lethal overdose or drug poisoning because of prohibition. Our American gulag is filled with mostly people of color and folks in marginalized communities because of the simple use or possession of a substance. I mean, these are catastrophic outcomes of prohibition. If anybody ever believed that prohibition was supposed to be helpful to vulnerable people, I think that’s been glaringly exposed as a terrible lie.” -Andrew
Harm Reduction Psychotherapy: A New Treatment for Drug and Alcohol Problems, by Andrew Tatarsky
Center for Optimal Living facebook
Centerforoptimalliving.com: Training + Events
Centerforoptimalliving.com: Integrative Harm Reduction Psychotherapy Certificate Program
The Hidden Dimension: Psychodynamics of Compulsive Drug Use, by Leon Wurmser
 Andrew Tatarsky, Ph.D. has worked with people who struggle with drugs and their families for over 40 years. He developed Integrative Harm Reduction Psychotherapy (IHRP) for treating the spectrum of risky and addictive behavior as an alternative to traditional abstinence-only substance use treatment. IHRP brings relational psychoanalysis, CBT and mindfulness together in a harm reduction frame and meets people wherever they are on their positive change journeys, working collaboratively to support people in discovering their truth and what goals and approach to positive change best suit them. The therapy has been described in a series of papers and his book, Harm Reduction Psychotherapy: A New Treatment for Drug and Alcohol Problems, which has been translated into Polish and Spanish and is currently being translated into Russian. He holds a doctorate in clinical psychology from the City University of New York and is a graduate of New York University’s Postdoctoral Program in Psychoanalysis and Psychotherapy. He is Founder and Director of the Center for Optimal Living in NYC, a treatment, education and professional training center based on IHRP. He is a member of the Medical and Clinical Advisory Panels of the New York State Office of Addiction Services and Support. He has trained individuals and organizations in 19 countries. His writing, teaching, clinical work and leadership aim to promote a re-humanized view of problematic substance use and a harm reduction continuum of care that will extend help to everyone who needs and wants it wherever they are ready to begin their positive change journeys.
Andrew Tatarsky, Ph.D. has worked with people who struggle with drugs and their families for over 40 years. He developed Integrative Harm Reduction Psychotherapy (IHRP) for treating the spectrum of risky and addictive behavior as an alternative to traditional abstinence-only substance use treatment. IHRP brings relational psychoanalysis, CBT and mindfulness together in a harm reduction frame and meets people wherever they are on their positive change journeys, working collaboratively to support people in discovering their truth and what goals and approach to positive change best suit them. The therapy has been described in a series of papers and his book, Harm Reduction Psychotherapy: A New Treatment for Drug and Alcohol Problems, which has been translated into Polish and Spanish and is currently being translated into Russian. He holds a doctorate in clinical psychology from the City University of New York and is a graduate of New York University’s Postdoctoral Program in Psychoanalysis and Psychotherapy. He is Founder and Director of the Center for Optimal Living in NYC, a treatment, education and professional training center based on IHRP. He is a member of the Medical and Clinical Advisory Panels of the New York State Office of Addiction Services and Support. He has trained individuals and organizations in 19 countries. His writing, teaching, clinical work and leadership aim to promote a re-humanized view of problematic substance use and a harm reduction continuum of care that will extend help to everyone who needs and wants it wherever they are ready to begin their positive change journeys.
 Juliana Mulligan has been an active member of the Ibogaine community for nine years and is currently working on her MSW at NYU. She runs Inner Vision Ibogaine, supporting people in preparation for, and in integration after treatment. She is also the Psychedelic Program Coordinator at the Center for Optimal Living. Previously Juliana was an opioid dependent person, and in 2011, with the help of Ibogaine treatment, she left opioids behind and set off on a path to transform the way drug users and their treatment are approached. She has been featured in DoubleBlind magazine, Chacruna, Woman’s Day magazine, and Psymposia.
Juliana Mulligan has been an active member of the Ibogaine community for nine years and is currently working on her MSW at NYU. She runs Inner Vision Ibogaine, supporting people in preparation for, and in integration after treatment. She is also the Psychedelic Program Coordinator at the Center for Optimal Living. Previously Juliana was an opioid dependent person, and in 2011, with the help of Ibogaine treatment, she left opioids behind and set off on a path to transform the way drug users and their treatment are approached. She has been featured in DoubleBlind magazine, Chacruna, Woman’s Day magazine, and Psymposia.
Instagram / Facebook / LinkedIn



In this episode of the podcast (and episode 3 of Vital Psychedelic Conversations), Kyle interviews Kylea Taylor: M.S.; LMFT; Grof-certified Holotropic Breathwork® practitioner; Vital teacher; and author of several books, including her newest, The Ethics of Caring: Finding Right Relationship with Clients (which you can win a signed copy of here).
She discusses her past and what she’s doing now, from learning breathwork from the Grofs at Esalen; to working through (and with) her 5-year spiritual emergency; to her work bringing breathwork to a residential substance abuse recovery program; to her InnerEthics® program, which she developed after realizing how traditional ethics education didn’t come close to covering the intricacies of working with non-ordinary states of consciousness.
They talk about how much the psychedelic community undervalues the reciprocity and knowledge one can gain from sitting for someone else; how a facilitator’s simplest question to ask when looking to intervene is, “Who’s this for?”; the need for therapists to have their own experiences and learn the territory of the medicines they’re using, how our multiple selves complicate already-complicated relationships, and three tools likely not yet mentioned in this podcast: Angie Arrien’s naming ceremony, SoulCollage®, and Brainspotting.
Plus, they talk about having dreams about taking psychedelics (have you ever had one?), and Kyle tells the story of his psychic dream – or as this show notes writer believes, his “making-prank-calls-while-sleeping” incident (sleep-pranking?).
“Informed consent is completely different, because how do you describe what a person is going to go into if they’ve never been into it? They’ve never had an extraordinary state of consciousness, let alone experience with that particular medicine. So you can describe it, but do they understand it? And can they really make an informed consent?”
“There’s exponential kinds of connections between the multiple selves, and it gets really confusing to sort out, so it’s another reason to know ourselves as well as we can, and to have experience in these states, and also to trust – when in doubt, go back to trusting the inner healing intelligence.”
“Therapists, with psychedelic-assisted therapy, need to be properly prepared and experienced, and know their scope of practice, and know themselves. I think trainings are doing a good job and we’ll get better as we go, but I think experience is the part that it seems like people are going to have to take care of themselves. If they really want to do the best they can for their clients, then they need to do it. We need to do it. We all do.”
The Ethics of Caring: Finding Right Relationship With Clients, by Kylea Taylor
Click here to win a signed copy of The Ethics of Caring!
Holotropic.com: “Doing Not Doing: A Facilitator’s Guide,” by Tav Sparks
Pathwaysvermont.org: Soteria House
Jungny.com: The concept of “Inferior function,” from Jung Lexicon, by Daryl Sharp
Psychedelics Today: PT288 – Annie & Michael Mithoefer – Vital Psychedelic Conversations
 Kylea Taylor, M.S., LMFT developed and teaches InnerEthics®, a self-reflective, self-compassionate, approach to ethical relationship with clients that she is now teaching in psychedelic psychotherapy trainings. Kylea started studying with Stanislav Grof, M.D. and Christina Grof in 1984 and was certified by them as a Holotropic Breathwork® practitioner in 1990. She worked with Stan Grof and Tav Sparks as a Senior Trainer in the Grof Transpersonal Training throughout the 1990s, and worked for nine years in a residential substance abuse recovery program. She is the author of The Ethics of Caring: Finding Right Relationship with Clients, The Breathwork Experience, Considering Holotropic Breathwork® and is the editor of Exploring Holotropic Breathwork®.
Kylea Taylor, M.S., LMFT developed and teaches InnerEthics®, a self-reflective, self-compassionate, approach to ethical relationship with clients that she is now teaching in psychedelic psychotherapy trainings. Kylea started studying with Stanislav Grof, M.D. and Christina Grof in 1984 and was certified by them as a Holotropic Breathwork® practitioner in 1990. She worked with Stan Grof and Tav Sparks as a Senior Trainer in the Grof Transpersonal Training throughout the 1990s, and worked for nine years in a residential substance abuse recovery program. She is the author of The Ethics of Caring: Finding Right Relationship with Clients, The Breathwork Experience, Considering Holotropic Breathwork® and is the editor of Exploring Holotropic Breathwork®.


In this episode of the podcast, Joe sits down with Co-Founder and CEO of Numinus, Payton Nyquvest, this time for a full episode (you may remember that he had a brief segment in Solidarity Friday #86).
Nyquvest tells the story of how ayahuasca became the cure for his chronic pain, and discusses pain in general and how we deal with it: how people so often fall into a box where their diagnosis becomes their identity, and how so much of healthcare is about alleviating the symptoms but never getting to the root cause.
He talks about how Numinus came about; how Health Canada’s Special Access Program could be huge towards more legalization; his concerns with the rush to ketamine and virtual therapy; patents and Compass Pathways; the importance of a safe container and community; and the need for a shift in how we view psychedelics and self work, from something we view as a last ditch resort to something we treat more as regular preventative tune-ups or check-ins.
Numinus is working with MAPS in their Phase 3 MDMA for PTSD study, and due to a license amendment by Health Canada that now allows them to produce a product from natural fungi, they have just produced what may be the first legal psilocybin mushroom since the 1970s.
“[I] saw this possibility [that] someone, through shifting their mental health and mental state, could greatly become a better version of themselves. And so, in my mid-to-late teens, became very, very passionate about mental health and my own mental health, and the intersection of mental health [and] physical health, and the recognition that you can’t compartmentalize the two. They’re all part of the same thing.”
“If you look at AA for example, there’s not a city on the planet I think that you could go to where you don’t find an AA community. And while certainly all these communities have their strengths and weaknesses, it really shows that with a really, really strong community, you can really help facilitate a lot of healing. …While the psychedelic experience is important, the integration and ongoing support and community is, I would argue, as important or more so.”
“I encourage everybody to read the results from the MAPS Phase 3 work, which is probably, I would argue, the most astounding clinical data we have on psychedelics for treatment-resistant PTSD, which, for anybody who doesn’t know; treatment-resistant PTSD is– this is a population of people who have tried every other treatment and have failed. Over 80% of people who went through the MDMA protocol saw a significant reduction in their symptoms and 67% actually no longer met the PTSD criteria after three treatments. That’s a cure for treatment-resistant PTSD, which is just an astounding thing to be able to say.”
The End of Alzheimer’s: The First Program to Prevent and Reverse Cognitive Decline, by Dale Bredesen
”Eyes on Oregon” YouTube Playlist
Psychedelicmedicinecoalition.org
 Payton Nyquvest is the Founder, Chair & Chief Executive Officer of Numinus, a company that empowers people to heal and be well through the development and delivery of innovative mental health care and access to safe, evidence-based psychedelic-assisted therapies. He has a deep understanding of the psychedelic industry from its infancy, driven by life-saving personal experiences with multiple therapy modalities. Additionally, Payton has deep business leadership experience, particularly in the finance sector, and is a recognized innovator and visionary in mental health care. At Numinus, he guides teams leading strategy, innovation, research and clinic network expansion, and supports the marketing and capital markets functions. He is responsible for raising more than $70 million for Numinus in the past year, and is quoted widely in media such as CTV, Forbes and the New York Times. In addition, he brings more than 15 years working in finance, investment and retail banking with some of Canada’s leading independent investment firms, including Jordan Capital Markets, Canaccord Financial and Mackie Research Capital. In these and other roles, he has raised more than $100 million for a variety of small cap companies.
Payton Nyquvest is the Founder, Chair & Chief Executive Officer of Numinus, a company that empowers people to heal and be well through the development and delivery of innovative mental health care and access to safe, evidence-based psychedelic-assisted therapies. He has a deep understanding of the psychedelic industry from its infancy, driven by life-saving personal experiences with multiple therapy modalities. Additionally, Payton has deep business leadership experience, particularly in the finance sector, and is a recognized innovator and visionary in mental health care. At Numinus, he guides teams leading strategy, innovation, research and clinic network expansion, and supports the marketing and capital markets functions. He is responsible for raising more than $70 million for Numinus in the past year, and is quoted widely in media such as CTV, Forbes and the New York Times. In addition, he brings more than 15 years working in finance, investment and retail banking with some of Canada’s leading independent investment firms, including Jordan Capital Markets, Canaccord Financial and Mackie Research Capital. In these and other roles, he has raised more than $100 million for a variety of small cap companies.
Instagram: @paytonnyquvest / @numinusinc
Twitter: @paytonnyquvest / @NuminusWellness
Linkedin: PaytonNyquvest / NuminusWellness
Facebook: NuminusWellness



“Education is not the filling of a pot, but the lighting of a fire.” – William Butler Yeats
The interest in psychedelics as a therapeutic tool is growing at a rapid pace, both by individuals looking for better solutions outside the current medical regime, and by practitioners looking for new and better ways to help their patients.
Even though regulatory systems lag behind, a paradigm shift in healthcare is clearly under way. The demand for safe, ethical, and effective treatment and integration is growing exponentially. Now more than ever, it is vital that educated, informed practitioners are ready and equipped to provide care when called upon.
After enrolling over 9,000 students in our eLearning platform and graduating over 500 in our eight-week, 47-hour program, Navigating Psychedelics, we’ve heard a lot about what people want and need from an in-depth training program – and also, what isn’t being offered out there. Our students have told us that training can be overly prescriptive, rigid, and clinical, with logistical hurdles and barriers to acceptance.
That’s where Vital comes in. Our new 12-month certificate program fills gaps in the current landscape of psychedelic training – both in course content and structure – and takes a holistic, experiential, and reflective approach to psychedelic practice and integration.
Vital was created by Psychedelics Today Co-Founders Joe Moore and Kyle Buller, M.S., LAC, and a team of people dedicated to helping others master the elements of psychedelic practice and contribute to the healing of the world. The culmination of over 15 years of work in psychedelic practice, the first Vital cohort of 100 students kicks off on “Bicycle Day,” April 19th, 2022.
Course content is packaged into five core modules, covering: psychedelic history and research; clinical therapies; the art of holding space; medical frameworks; and integration theories and techniques. Each comprehensive module spans between seven to ten weeks of specialized lectures led by guest expert teachers as well as more intimate study groups facilitated by our instructors.
The best teachers are those who show you where to look, but don’t tell you what to see.
-Alexandra K. Trenfor
Over the years, Psychedelics Today has developed relationships with a humbling number of leading researchers, historians, clinicians, and bright minds working in research and application, advocacy, spiritual practice, and patient care. We’ve assembled some of the very best to work with Vital students, including:
View the full list of instructors here.
We believe that no amount of learning from clinical studies, reading textbooks, or listening to an instructor can make up for first-hand experience with holotropic states. Furthermore, we believe openness and sharing of experience validates clinical evidence, helps inform research and the approach to patient care, and helps undo stigma and misguided perceptions caused by the war on drugs.
Throughout the course, students will be challenged to deepen their personal understanding of psychedelics and reignite their transformation by attending one of six experiential retreats (in either the United States or abroad). Stay tuned for more details on dates, locations and pricing.
While the deeply experiential nature of the course supports the growth of practitioners, the course is also designed to equip participants with the knowledge they need to establish a psychedelic-informed practice from the ground up. For coaches, facilitators, mental health and complementary health practitioners, Vital provides a thriving community of specialists to support their mission.
Fair access to psychedelic medicine begins with fair access to essential education. In addition to flexible payment plans for all students, we’ve committed to provide scholarships for 20% of students from each cohort, sponsoring up to 100% of tuition to support their mission.
Scholarships are awarded on a case-by-case basis, and are reserved for people who:
At the end of the program, graduating students receive a certificate in Psychedelic Therapies and Integration. CE credits will be offered, but stay tuned for more details.
Full details on scholarships and credits are in the extended course brochure, available on the Vital website.
Program registrations are open now, and close at midnight EST on March 27th. Acceptance will be offered based on eligibility and order of submission (with priority to students receiving scholarships). Once all seats in the initial cohort are filled, subsequent approved students will be placed on a waitlist and invited to join the course when a spot becomes available. Interested students are encouraged to apply as soon as possible. Apply here.
For more information on Vital and how to register, visit the program website or connect with our team at Vital@psychedelicstoday.com.
Link to press release
Gathering as professionals in psychedelics has taken on new meaning. It’s more – a lot more – than just networking now.
In early December, Horizons: Perspectives on Psychedelics (an annual conference often referred to just as ‘Horizons’) re-emerged from the proverbial ashes of COVID-19; a pandemic that led to the dismantling of social connectivity and a general feeling like we were moving with momentum. With the pandemic came distance: social distance, emotional distance, and psychological distance. We stopped going to work together, we stopped learning together, we stopped moving and growing together. Reconvening at Horizons was therefore much more significant than just attending a regular conference.
Pandemic or not, the Horizons conference already played the role of a psychedelic sandbox where the psychedelic community convenes each year – a place where we get to see how widespread the community really is, and where each conversation is an opportunity to learn from our peers. It is a place where we can learn together, cry together, break bread together, and dance together. It is a place where we can be our most authentic selves, see others, and be seen. And it is a place where difficult conversations are encouraged to be had.
I heard a colleague explain that at other conferences, we are often introducing psychedelics to a new audience that sometimes lacks the capacity to grasp the shadow of psychedelic therapy. Contrarily, Horizons seeks to shed light on our shadow. It seeks to broaden our collective dreams of what is possible in the psychedelic space while learning from our past. By having those difficult conversations in front of 2,000 people, we get to grow collectively – as a community, and as a movement. And this year’s Horizons, more than ever, was an opportunity to rebuild a sense of collective effervescence.
Sociologist Emile Durkheim coined the term “collective effervescence“ as a “shared state of high emotional arousal related to intensification of emotions by social sharing, felt in religious and secular collective rituals, irrespective of their content (joyful feasts or sad funerary rituals), which empowers the individual.” Essentially, collective effervescence occurs when there is a shared sense of engagement with something bigger than the self, warranting a personal sense of empowerment. In developing the Perceived Emotional Synchrony Scale, psychologists Anna Wlodarczyk, Larraitz Zumeta, and their fellow researchers determined that some of the key conditions for collective effervescence to emerge are a “shared attention on one or more symbolic stimuli” and a sense of “intentional coordination or behavioral synchrony among the participants in a given gathering.” Ultimately, they argued that “the relevance of emotional synchronization in collective gatherings [is] conducive to strong forms of social identification, particularly the overlapping of the individual with the collective self.”

By blurring the lines between the individual and the collective self, Wlodarczyk and her colleagues suggested that a sense of collective effervescence ultimately “pulls humans fully but temporarily into the higher realm of the sacred, where the self disappears and collective interests predominate.” It is no surprise that a conference discussing the ethics and future of the psychedelic movement would incite a collective effervescence so strong that a perceived sense of emotional synchrony may occur, where there is indeed a “co-present other” that becomes closer and closer to a perceived sense of self.
This is how I want to see the psychedelic movement evolving and growing, with the collective interest dominating a sense of self. The uniqueness and radicalness of this movement will only come from our ability to enter into this shared sense of togetherness, and into a “higher realm of the sacred” and not to bypass it. How can we do this?
“Shadow work” is a term those in the psychedelic movement have heard countless times. In psychedelic healing, shadow work is not about eradicating the shadow. Rather, it is about shedding light on it and getting to know it deeply, so that when it shows up, it is not unfamiliar. By working with the shadow, we become better equipped to handle what may come up as a result of trauma. If we do not have a safe space to have these conversations, to be held in our confusion, and to be educated on our blind spots, then how can we move forward? How can we call ourselves a revolution if we are not rethinking the way we engage with our work each and every year?
Horizons is a place where we learn about cutting edge research in science and in the clinic, new models for approaching business, and cultural matters. But more importantly, it’s an opportunity to converge as a community and reflect on the previous year together, shedding light on our blind spots and engaging in shadow work to build a sense of collective effervescence and a unified goal. While there were many great presentations this year, three in particular really encapsulated all of this.
Without a doubt, the most impactful talk of the weekend for me was from marriage and family therapist, Laura Mae Northrup, who, in light of recent events, spoke about sexual misconduct in the psychedelic space. Shivers ran down my spine as she powerfully proclaimed these words into the microphone: “Mental health clinicians self-report engaging in sexual violations with their clients at rates of 7-12%. We don’t have data on corresponding rates of psychedelic therapies, but we have no reason to believe it would be any less than our non-psychedelic counterparts.” She spoke with conviction, with grace, and emotion. She had us all in tears, reflecting on the very real fact that the clinicians who are at a higher rate of sexually abusing their clients are male clinicians who were sexually abused as kids.
Northrup highlighted that we are in a cycle of abuse; that healing trauma is painful, and without doing so effectively, we will continue to cause harm to others. She did not name names, and she did not stand on that stage building a pedestal for herself (regardless of how compelling it seemed, as she noted). Instead, she served her community and said what needed to be said. If there was one takeaway from her powerful talk, it was that “we need to heal ourselves.” She took what was frantically scrambling around everyone’s minds and hearts, and put it into powerful and sensical words. She made it make sense.
Tears continued to flow down my face as Horizons founder Kevin Balktick approached the podium, applauding Northrup for the outstanding courage it took for her to get on that stage and speak from her heart. He then declared that sexual abuse and misconduct should not be a “women’s issue”; that it always has, and certainly should be, a men’s issue as well.

The second presentation that captivated my attention was from ibogaine treatment specialist, Juliana Mulligan, who spoke of her experience of being sent to jail for using heroin, being thrown on the streets in the middle of Bogota, Colombia, and finally seeking refuge in what she was told was a miracle “cure” for opioid dependence. She then shared her own horrifying journey of getting off of opioids by going to an ibogaine center that did not have the proper protocols in place.
She brought about gasps in the crowd when she told us that the clinic did not have a heart monitor and that they gave her twice the safe dose of ibogaine – certainly enough to kill anyone, she clarified. When the clinic noticed her abnormal EKG readings and decided to seek professional and medical help, she was refused by three hospitals largely due to a lack of understanding on how to handle her situation, being overwhelmed with patients, and not believing that someone her age could be having a heart problem. Finally, when the fourth hospital almost turned her away, she had her first of six cardiac arrests due to her high dose of ibogaine. She explained that she remembers very little about her experience on ibogaine, but that she woke up with a tiny fraction of the usual opioid withdrawal symptoms, the feeling of a huge weight lifted from the guilt and shame of years of substance use, and a newfound clarity around her life’s mission.
Despite her experience at this ibogaine clinic, Mulligan has not turned her back on the promise of ibogaine in treating opioid dependence. In fact, she has dedicated part of her career to ensuring that people are equipped with the tools and knowledge on how to choose an ethical and effective ibogaine clinic – something she realized was necessary due to the many vulnerable people who don’t know what to look for when choosing an ibogaine clinic. Often, people do not take the time to learn about the proper protocols needed to provide this treatment, with many acting out of desperation in an attempt to “fix” their issues as quickly as possible. Her main point was to remind us of the dangers of selling ibogaine as a “miracle cure,” and how damaging it can be for people to have the idea that Ibogaine will fix their issues overnight.

Finally, ex-convict William Leonard Pickard held us all in a state of awe as he eloquently and captivatingly shared his story of spending 21 years in prison for allegedly producing 90% of the United States’ supply of LSD. He spoke softly, and took long pauses between his sentences, his descriptive tone allowing me to truly visualize the scene where a CIA agent pointed a rifle at his forehead while uttering, “I’m going to blow your brains out.” He told us about the violence that occurred in prison, and how he became desensitized to fights and killings while he would quietly sit and eat his lunch. He showed us photos of a prison cell, and told us about how he fell in love with American Literature, and that without that – coupled with deep meditation, he may have not survived.
Pickard reminded us all why we were sitting in that room and why we need to change the way psychedelics have been viewed since the 1970s. The majority of the people in that room are privileged enough to never experience going to jail for psychedelics, and getting a glimpse into that reality reminded us why rewriting the psychedelic script in America is critical.
In exploring rituals where collective effervescence is powerful, Wlodarczyk and her team discuss the way in which both positive and negatively valenced rituals ultimately lead to a shared sense of emotion and heightened well-being. Indeed, what truly comes through in these rituals is “the creation of a positive emotional atmosphere in which grief, sadness, anger, and fear are transformed into hope, solidarity, and trust.”
Contextualizing these experiences –sexual misconduct in psychedelic healing, the wrongful advertisement of ibogaine as a miracle cure, and the harsh realities of the drug war and the American justice system – provides our collective community with the opportunity to transform these emotions of grief, sadness, anger, and fear into a shared sense of solidarity. We were provided with the opportunity to compost these moments of disappointment and turn them into something productive, where the unified goal of ethically bringing psychedelics to modern American lives empowers each and every one of us, both on a collective and individual level. This is how we can heal and move forward as a collective movement.
These three presentations are simply a glimpse into the moving stories that were told on that stage. The breadth of content shared allowed us the opportunity to reflect on what the world could look like once we systematically dismantle the war on drugs, and what is effectively involved in doing so: the clinical trials for which researchers have put their careers on the line, the endless volunteer hours that policy makers and lawyers have been putting toward changing legislation, the repairing of relationships with Indigenous communities through the work of the Native American Church and the Religious Freedom Restoration Act, the importance of doing our own work in order to help others heal from their trauma, and the dangers of presenting psychedelics as a magic bullet.
There are many pathways to attain psychedelic healing. Horizons provides a space for the entire range of themes that ought to be considered in bringing psychedelics to the modern world. In order to achieve this goal, we must do so collectively. We must reimagine what it means to be successful, and we can only do this by building a collective sense of self. To do this, we must continue to have these conversations, processing fear and anger into hope and solidarity. If we want to see the psychedelic movement radically change the world we are living in, we must face the music by continuing to have these difficult conversations and seek to elevate collective effervescence.
In this episode of the podcast, Kyle and David interview Andrew Penn: nurse practitioner, Co-chair for Sana Symposium, Associate Clinical Professor at the University of California–San Francisco School of Nursing, and Co-founder of OPENurses; a professional organization for nurses interested in psychedelic research.
Penn discusses how he came into the world of psychedelics and how in his early days, the only way to talk about psychedelics for therapeutic use was in a sidebar to speeches on drug abuse. He talks about reframing that conversation, the progress he’s seen, why psychedelics and SSRIs may actually work together, microdosing and the placebo effect, how the placebo effect may play into other aspects of healthcare you might not have thought about, why psychedelics needs more skeptics, and the importance of care in healthcare.
He talks about OPENurses (The Organization of Psychedelic and Entheogenic Nurses), which he co-founded to make sure more nurses are involved (and front-facing) in the psychedelic space. He feels that nurses are more prepared for psychedelic treatment than other professions, but the biggest hurdle they’ll face will be learning when to not intervene and just let something play out (something that’s very common in psychedelic therapy but not at all in traditional medicine).
And lastly, he talks about how we need to stop romanticizing the idea that you need to have a huge experience with re-lived trauma in order to heal, and that we should have an appreciation for the subtle – that change is gradual, and often it’s more about creating a better relationship with the thing we can’t change than eliminating it.
“Back in those early days, the only way I could talk about psychedelics was, essentially, embedded in a talk about drug abuse. In fact, the very first time I talked about MDMA as a therapeutic agent was in a talk about bath salts.”
“I think it’s interesting that as a community of people who really are not necessarily rational materialists – you know, we’re not necessarily mechanistic in our way of thinking – that people get really mechanistic about microdosing; that it’s like, ‘Oh, it’s this tiny little dose of LSD or whatever that is making this change.’ And I’m a little puzzled why people want to essentially take a regular dose of a psychedelic. I mean, how is that any different than taking a regular dose of Fluoxetine or Lexapro or something like that? I just don’t see it as being that radical, quite honestly. …LSD is not a naturally-occurring compound. It has to be synthesized. So does Fluoxetine. I mean, maybe psilocybin, but I’m just a little puzzled by the phenomenon.”
“I think psychedelics needs more skeptics, honestly. I think we either have to bring the skepticism ourselves, or other people and other forces who are not as convinced as people in the psychedelics community will do it for us. I used to have a therapist years ago who liked to say, ‘Do you want to be uncomfortable on your terms or on somebody else’s?’. And I think that’s a great question that the psychedelics field could ask themselves, because if we don’t bring this level of scrutiny and skepticism to our work, then other agencies like the FDA will.”
“When you’re trained in healthcare, we’re often explicitly taught (or implicitly taught) that we need to do something; you know, what’s the intervention? What’s the thing you’re going to do? And often in psychedelics, the thing to do is to hold still. …I think the drive to intervene is well-intended but often, ultimately can be incorrect. What we all need to learn (not just nurses, but just all of us in this profession) is that sometimes the right answer is to watch this unfold. Choosing not to intervene is actually an active process.”
The Doors of Perception and Heaven and Hell, by Aldous Huxley
Core Concepts of Jean Watson’s Theory of Human Caring/Caring Science
Psychedelics Today: PT231 – Dr. Hassan Tetteh – Human Care Over Health Care
Chacruna.net: How I Joined the Secret SSRI Circles of 1985
Pubmed: Depression Is the Leading Cause of Disability Around the World
American Journal of Nursing: Supporting the Patient on LSD Day (from 1964)
American Journal of Nursing: CE: Psychedelic-Assisted Therapy (their follow-up)

Andrew Penn, NP was trained as an adult nurse practitioner and psychiatric clinical nurse specialist at the University of California, San Francisco. He is board certified as an adult nurse practitioner and psychiatric nurse practitioner by the American Nurses Credentialing Center. He has completed extensive training in Psychedelic-Assisted Psychotherapy at the California Institute for Integral Studies and recently published a book chapter on this modality. A leading voice for nurses in psychedelic therapy, he is a cofounder of OPENurses, a professional organization for nurses interested in psychedelic research and practice and was a study therapist in the MAPS-sponsored Phase 3 study of MDMA-assisted psychotherapy for PTSD and is a Co-I in the Phase 2 Usona sponsored study of psilocybin-facilitated therapy for major depression. Additionally, he is a co-author in a recent article in the American Journal of Nursing on psychedelic assisted therapies, the first in 57 years. He is the Co-chair for Sana Symposium, a leading national CME meeting on psychedelic therapies.
Currently, he serves as an Associate Clinical Professor at the University of California-San Francisco School of Nursing and is an Attending Nurse Practitioner at the San Francisco Veterans Administration. He has expertise in psychopharmacological treatment for adult patients and specializes in the treatment of affective disorders and PTSD. As a steering committee member for Psych Congress, he has been invited to present internationally on improving medication adherence, cannabis pharmacology, psychedelic-assisted psychotherapy, grief psychotherapy, treatment-resistant depression, diagnosis and treatment of bipolar disorder, and the art and science of psychopharmacologic practice. He also keeps regular blogs on all things psychiatric and has been interviewed in Forbes, the Los Angeles Times, and on the BBC World Service.



In this episode of the podcast, Joe interviews Chairman and Chief Executive Officer of Tryp Therapeutics, Greg McKee.
Tryp Therapeutics, a fairly young, early-stage biotech company, is focusing on nociplastic pain (the hard-to-explain pain where nothing seems physiologically wrong, but a nerve signal related to pain seems to be stuck in the “on” position) and how it could be alleviated through the rewiring often possible in the psychedelic experience. They are first looking at psychedelics for chronic pain and eating disorders, and when this podcast was recorded, had just received FDA clearance to begin a fibromyalgia study at the University of Michigan (with studies on phantom limb pain, complex regional pain syndrome, binge eating disorder, and hypothalamic obesity likely coming after). They are also working on a psilocybin derivative-based novel compound and novel route of administration/protocol, possibly with the ability to stop a difficult trip when necessary.
McKee discusses the origins of Tryp, the benefits of using synthetics, 5-MeO-DMT, how the Nixon administration killed research progress, the positives to take away from Compass Pathways’ preliminary psilocybin Phase 2B trial results, MAPS and possible insurance models, Robin Carhart-Harris, why a lot of early psychedelic investors may be mistakenly panicking, and the idea of insurance covering the treatment of a patient for a period of time rather than number of visits.
“We think that there’s a huge opportunity to unleash the full potential of psychedelics, well beyond traditional mood disorders.”
“It’s a fascinating field, no doubt. There’s a lot to be learned and there’s still a lot more questions, frankly, than answers. That’s the thing that’s really quite surprising. I mean, I’ve been on a learning curve [and] I got right to the edge fast, because I realized, ‘Oh shit, nobody has the answers to these questions.’”
“The thing about synthetic is that it just allows you not only to have consistency and all that that we just [talked] about, but it allows you to scale so you can impact so many other people’s lives. So it is a little bit of a pain in the backside to go through this process, and I can totally get why certain people are saying, ‘Hey, why do we need the pharma industry to do this?’, but on the other hand, if life science investors and biotech and pharma companies do get involved and push this through to market; boy, you’re going to be able to treat so many more patients.”
YouTube: Stanislav Grof: Psychedelics and the Future of Humanity, from Psychedelic Science 2017
Psychedelics Today shop: Save a Toad Short-Sleeve Unisex T-Shirt (it’s “exploit a chemist,” not “squeeze,” Joe)
Chasing the Scream: The First and Last Days of the War on Drugs, by Johann Hari
University of Michigan: Chronic Pain & Fatigue Research Center (where Dr. Dan Clauw works)
Psychedelics Today: PT245 – Robin Carhart-Harris – Psychedelics, Entropy, and Plasticity
 Greg McKee serves as Chairman and Chief Executive Officer of Tryp Therapeutics. Greg has served in executive management positions for more than 20 years. He started his career in life sciences with Genzyme before serving as Chairman and CEO of publicly traded Nventa Biopharmaceuticals. Greg also served as CEO of CONNECT, a startup accelerator, and as Co-founder and Managing Director of Torrent Ventures. Greg earned a BA in economics from the University of Washington, an MA in international studies from the University of Pennsylvania, and an MBA from the Wharton School. He has worked in Tokyo for seven years and has been a member of YPO since 2006.
Greg McKee serves as Chairman and Chief Executive Officer of Tryp Therapeutics. Greg has served in executive management positions for more than 20 years. He started his career in life sciences with Genzyme before serving as Chairman and CEO of publicly traded Nventa Biopharmaceuticals. Greg also served as CEO of CONNECT, a startup accelerator, and as Co-founder and Managing Director of Torrent Ventures. Greg earned a BA in economics from the University of Washington, an MA in international studies from the University of Pennsylvania, and an MBA from the Wharton School. He has worked in Tokyo for seven years and has been a member of YPO since 2006.



In this episode of the podcast, Joe interviews Clinical Professor at the University of Florida, College of Pharmacy: Oliver Grundmann, Ph.D.
While Grundmann’s focus is the neuropharmacology of natural products in general (especially those with potential for dependence), this episode is entirely about a substance that has been mentioned on the podcast, but never fully dissected: Mitragyna speciosa – otherwise known as kratom.
And they cover it all: What to look for when purchasing kratom; possible risk factors and drug interactions; the contaminants most often seen; its history with the FDA; its safety profile; what the veins mean when people describe kratom as “red vein;” what is being researched today; what an alkaloid is; how to safely explore kratom and monitor dosing; what the future could hold; and of course, the science behind how it works. Get ready for mitragynine, 7-hydroxymitragynine, and the μ-opioid receptor to be part of your vernacular!
Grundmann is currently analyzing Top Tree Herbs‘ products to see how they differ from others, specifically looking at how much mitragynine people are actually getting when drinking a tea dissolved in water (vs. levels from the whole plant dissolved in methanol, which most current research shows). He believes more real world evidence could help push kratom in the direction of being considered a dietary supplement. If you use kratom and want to add to the conversation, you can fill out his questionnaire here.
“You tell the FDA something acts on the opioid receptor and they see, immediately: Oh my gosh, we’ve got something else that might contribute to the opioid epidemic. I think that was kind of the concern of the FDA, which is a legitimate concern, but I think, as you pointed out; there is more to the story. You need to look at the whole picture.”
“If somebody who has used alcohol for years in advance is then using kratom and shows signs of liver injury or failing liver, then contributing that to relatively recent kratom use appears to be a stretch. But yet, it is being done in the literature.”
“It doesn’t necessarily always have to be an illicit use of the drug. It can be that somebody was completely, legitimately prescribed an opioid (a benzodiazepine) and then they did not feel adequate symptom relief and they added kratom to it. And the self-treatment of kratom then resulted in a potential drug interaction that led to a fatality. Does that mean that kratom was the causative agent? That is the problem, since we do not know exactly what the effects of kratom are.”
Pharmacy.ufl.edu: Oliver Grundmann, Ph.D.
His anonymous kratom questionnaire
Pharmacy.ufl.edu: Kratom tea study stirs up new support for relieving opioid dependence
Pubmed: The pharmacology and toxicology of kratom: from traditional herb to drug of abuse
Americankratom.org (American Kratom Association (AKA))
Pharmacy.ufl.edu: NIDA awards UF College of Pharmacy additional $3.4 million kratom grant
 Dr. Oliver Grundmann is a clinical professor at the University of Florida, College of Pharmacy. He serves as the Director of the graduate programs in Pharmaceutical Chemistry and Clinical Toxicology, is a fellow of the American College of Clinical Pharmacology, and his primary research interest is centered on the neuropharmacology of natural products, especially substances with potential for tolerance and dependence development. He has authored over 75 publications, 5 book chapters, and given over 40 presentations at national and international conferences. Dr. Grundmann obtained his BS in Pharmacy from the Westfälische-Wilhelms-Universität Münster in Germany, and his Ph.D. in Pharmaceutical Sciences, MS in Forensic Toxicology, and MEd from the University of Florida. He has been teaching on the subject of natural products, drug abuse, forensic & clinical toxicology, and pharmaceutical sciences for the past 13 years.
Dr. Oliver Grundmann is a clinical professor at the University of Florida, College of Pharmacy. He serves as the Director of the graduate programs in Pharmaceutical Chemistry and Clinical Toxicology, is a fellow of the American College of Clinical Pharmacology, and his primary research interest is centered on the neuropharmacology of natural products, especially substances with potential for tolerance and dependence development. He has authored over 75 publications, 5 book chapters, and given over 40 presentations at national and international conferences. Dr. Grundmann obtained his BS in Pharmacy from the Westfälische-Wilhelms-Universität Münster in Germany, and his Ph.D. in Pharmaceutical Sciences, MS in Forensic Toxicology, and MEd from the University of Florida. He has been teaching on the subject of natural products, drug abuse, forensic & clinical toxicology, and pharmaceutical sciences for the past 13 years.



In this week’s Solidarity Fridays episode, we tried to have a 2-parter, but like many things in 2021, that just didn’t quite go as planned. Hopefully, the Compass Pathways patent analysis (with patent attorney Stefan J. Kirchanski) can be re-recorded for a future episode. Stay tuned…
In the part that was successfully recorded, Joe and Kyle highlight some recent news: most notably the emergence of the Natural Medicine Healing Act, which will allow Colorado voters to decide whether or not to legalize possession and personal cultivation of ibogaine, DMT, non-peyote-derived mescaline, psilocybin, and psilocyn up to 4 grams (of the actual drug, meaning 4 grams of psilocybin, not 4 grams of mushrooms containing psilocybin), as well as establish “healing centers,” where adults could receive treatment from trained facilitators.
They then cover the University of Texas’ Dell Medical School opening a center to study psychedelics, YouTube user Psyched Substance’s recent admission that his drug use had gotten out of hand and he has quit everything, and Colorado health leaders working to establish specific guidelines around how police, paramedics, and EMTs handle ketamine – which obviously needs to happen after Elijah McClain’s 2019 death from being forcibly given entirely too much.
Also discussed: drug exceptionalism, Carl Hart, Run Ronnie Run!, and how much having family involved in ketamine-assisted therapy could help with the process (even if they have absolutely no understanding of it).
“Yes, decriminalizing psychedelic compounds is a step in the right direction. To me, it’s not a holistic step, because we’re still putting people in jail.” -Joe
“We do need situations like this with really weird drugs like ketamine. …Are the authorities using it properly? And I think this is a good sign that, in some cases, even though it’s years late, we can improve drug policy.” -Joe
“You have this massive transcendent experience. Who’s to say your friends, family, and people you’re around are going to have any way to relate to that, especially a way that’s positive for you?” -Joe
Drug Use for Grown-Ups: Chasing Liberty in the Land of Fear, by Dr. Carl L. Hart
Chasing the Scream: The First and Last Days of the War on Drugs, by Johann Hari
Update: Man Jailed for Joint Set Free (Joe, he’s been set free!)
Huffpost.com: This Man Is Serving More Than 13 Years In Prison Over Two Joints’ Worth Of Marijuana
Statesman.com: Dell Medical School starts center to study psychedelics for mental health treatments
Psyched Substance YouTube: My Family Left Me. I Was WRONG About Psychedelics.
9news.com: State panel makes recommendations for safe ketamine usage
9news.com: Two paramedics each face 11 charges in connection with the death of Elijah McClain.



In this episode, Joe interviews seventeen year veteran of federal policy, past Navigating Psychedelics student, and founder of Healing Equity and Liberation (HEAL) Organization, Micah Haskell-Hoehl.
Haskell-Hoehl talks about growing up in Pittsburg and seeing disparities in how the school system treated him in comparison with people of color, discovering psychedelics and their healing potential, his path to federal policy and creating HEAL Organization, and his realization that psychedelics can not only help heal deep wounds, but also do something less talked about when considering race relations: help white people deal with how they fit into a culture founded in colonialism and white supremacy. He also discusses the nuance in patenting and IP; how private companies have financially benefited from taxpayer dollars; and how, while he’s excited for the future, he’s worried that mental health disparities will get even worse in the coming corporate wave if these medicines are only available to the rich and connected (or if policymakers aren’t thinking of everyone).
Through HEAL Organization, he’s working to gather evidence that proves to providers that it makes financial sense to cover all types of psychedelic therapy, get public funds allocated to give everyone access, and fix barriers so people have the time and resources necessary to work with these medicines. He has worked with the Plant Medicine Coalition to create the National Council on Federal Psychedelics Priorities to collect like-minded individuals and organizations, figure out exactly what psychedelic policy should look like, and take the first steps to get this (unfortunately slow-moving) process going.
“From as early as I can remember, [I] can recall thinking there’s not that big of a difference between these kids and [me]. We’re all human. We’re all very much the same. So there’s something going on here that is warping our experiences and our life trajectories, and that’s external to who we are as individual people.”
“As a white guy, I know my experience, and I just want to say that I think that there’s really tremendous possibilities out there for white people to deal with our racial shit through psychedelic healing as well. So you know, there’s the whole concept of white fragility and the shirking away of confronting issues of race and systemic oppression; that is a common experience for white people. The way that we, I think, as white people, have internalized trauma that is premised on white supremacy as well. …Psychedelic healing is a real amazing opportunity for us to dig at those issues in ourselves, because the systems of oppression operate external to us, but also through us, and exist inside of us too.”
“I just don’t believe that psychedelic healing can reach its full potential inside of this broken social container where these systems of oppression are just running roughshod over entire communities of people. I just fail to see how that’s possible. So I think as a movement, I would challenge folks to think about why it’s psychedelic to promote a full end, hard stop to the war on drugs.”
Instagram: @healing_equity_and_liberation
Slate.com: Jonas Salk: Good at Virology, Bad at Economics
Leaps.org: Meet the Psychologist Using Psychedelics to Treat Racial Trauma
The People of Color Psychedelic Collective
Lawenforcementactionpartnership.org (LEAP)
 Micah is the founder of Healing Equity and Liberation–or HEAL–Organization. It is working to create a justice framework for psychedelic decriminalization, regulation, and healing, using federal policy. He’s worked in federal policy for nearly two decades, including at Vera Institute of Justice and the American Psychological Association. Micah’s both found healing from depression through the use of psychedelics and struggled with substance use, for which he’s been in long-term recovery for over eight years.
Micah is the founder of Healing Equity and Liberation–or HEAL–Organization. It is working to create a justice framework for psychedelic decriminalization, regulation, and healing, using federal policy. He’s worked in federal policy for nearly two decades, including at Vera Institute of Justice and the American Psychological Association. Micah’s both found healing from depression through the use of psychedelics and struggled with substance use, for which he’s been in long-term recovery for over eight years.



Our understanding of the brain in the 1800s was quite different from what we know today – and pretty weird, too.
You can’t throw a tab of LSD without hitting a story about psychedelics these days. While psychedelics are going through a scientific renaissance, 150 years ago, the field was a circus of misinformation and racism. Occasionally though, through that potpourri of misguided madness, it nailed some concepts that still hold up today. Granted, future scientists will most likely write an article clowning the state of psychedelics in the early 2000s to today, but let me be the first to start that vicious cycle by highlighting some of the more ridiculous concepts people believed in the 19th Century.
While there may have been many ethnographic studies of psychedelics dating back to the Bronze Age, the concept of modern neuroscience is a fairly new field. In the 1880s, the interest in neuroscience formed from humanity’s attempt to explain mental illness and addiction through scientific terms as opposed to supernatural spirits possessing bodies. Some neuroscientists in the 19th century believed a person’s cognition, along with predisposition of behavioral traits was rooted in neuroanatomy, which some believed was reflected in the physical structure of the skull. The idea that chemistry played a role in brain functionality was a novel concept that didn’t have much support in the scientific community in the early 1880s. In fact, the closest thing science got to neurochemistry was in 1809, when Johann Christian Reil soaked a brain in pure alcohol for a week just to see what would happen (if you’re wondering, it got really hard and took on the texture of shoe leather).
To first understand the state of neuroscience in the 1800s, we must first comprehend the state of science at the time, and it was bonkers.
The idea that all living organisms consisted of cells and that all cells originated from pre-existing cells (cell theory) proposed by German physiologist Theodor Schwann in 1839 was revolutionary. It shifted the deeply-held religious belief that life originated supernaturally, and instead, emerged from biological means. It sounds trivial now, but society took a collective seat and came to the realization that each person was a community of cells working in unison to create a ‘Bob,’ Connie,’ or ‘Karen’ (and of course, all those Karen cells wanted to see the manager shortly after being created).
Twenty years after the world recovered from Schwann’s cell theory, Darwin dropped The Origin of a Species, giving birth to the concept of evolution, a radical idea that once again shifted humanity’s focus away from divine creation and more closely towards the modern worldview we hold today.
Science in the 1800s was also notoriously racist. Many people used Darwin’s evolutionary theory to justify hateful pseudoscience that revealed the most vile aspects of humanity. While he was able to consciously remove himself from the 19th century racism that prevailed in science at the time, most could not. Franz Joseph Gall constructed the basic ideologies of phrenology in 1808, which was a belief that a person’s mental aptitude could be determined by bumps and ridges in a person’s skull — evidence Gall believed was the pressure of the neuroanatomy of the brain on the skull. More specifically, he believed a person’s behavior was localized in different compartments in the brain — a total of 28 areas to be exact. Things like ‘the firmness of purpose,’ ‘love of poetry,’ and even a place in the brain that’s responsible for a person’s tendency to murder, Gall insisted, could be determined through cranial anatomy.
When phrenology emerged in Europe in the 1800s, most scientists discarded the idea since its foundations were based on faulty neuroanatomical information. Gall was tossed out of Austria for proposing such an obviously absurd idea and eventually ended up in France, where even Napoleon Bonaparte ridiculed his concept of phrenology. When the rest of the world seemed to collectively reject phrenology as the pseudoscience it truly was, it found a home in America — because at that conflicted time, obviously it would.
With abolitionist movements spreading across the country along with the social underpinnings of what would be known as the Civil War, phrenology was used as a “scientific” reason to justify slavery in America and the overall disgusting treatment of Indigenous people as land continued to be removed from tribal territories. However, phrenology did have its fierce opponents, like John P. Harrison, editor of the Western Lancet, a peer-reviewed medical journal that caught the attention of Southern political leaders when it was introduced to America (and is still in print today). With the assistance of books like Phrenology Vindicated by Charles Caldwell and Crania Americana by Samuel Morton, political leaders had the “scientific” backing to make absurd claims like Africans were neurologically designed to be enslaved and Indigenous Americans were biologically a different species than white people — which made stealing their land a natural process ordained by God.
Amongst the incendiary nature of science during the 19th century, the unlikely emergence of psychedelic neuroscience occurred — and like all things in the 1800s, it was undoubtedly a product of its time. That’s a nice way to say it was sometimes wrong and mostly racist, but interestingly enough, it got some things right.
Neuroscience can be defined as the objective study of the brain and the central nervous system. The first neuroscientist to analyze the effects of psychedelics was Germany’s Louis Lewin in his book, Phantastica. Although it was officially released in 1924 when Lewin was 74, it contained his collected psychedelic research that took place in the late 1800s. Among the many drugs he categorized, he decided not to call psychedelics “hallucinogens” since not all substances elicit a hallucinatory response. “Phantastica” was the word he decided on, along with other equally interesting names like “Inebriantia” for drugs like alcohol, and my personal favorite, “Excitantia” for substances like caffeine and nicotine.
Lewin was never really a scientific rock star in his time though, mostly because he refused to renounce his Jewish heritage in 19th-century Germany – racism and anti-Semitism in the scientific community at this time went hand-in-hand. However, Lewin did get the props he deserved in psychedelics when Paul Henning of the Berlin Botanical Museum named peyote Anhalonium Lewinii in Lewin’s honor.
Around the time Lewin came on the scene, most people were describing psychedelics in a subjective manner, wrapped up in pseudo-science and religious mysticism. People weren’t tripping because of psychedelic-induced neurological activity — evil spirits possessed the taker of the psychedelic, which meant evil behavior was soon to follow. Metaphysics, with its focus on the nature of human consciousness and existence, was rapidly growing in the 1800s. Lewin believed that describing psychedelics in metaphysical terms would ruin what we could potentially learn from them. His research was wholly focused on dispelling the pseudoscience that surrounded psychedelics, yet Lewin fell into the trap of anointing psychedelics with otherworldliness with his idea that an invisible force called ‘vital energy’ surrounded all living things. Lewin believed this vital energy governed all chemical, mechanical, and physical properties of each person and that psychedelics had the ability to interrupt this energy. He also believed a person’s resistance to psychedelics was dependent on the strength of their vital energy.
This wasn’t the first time Lewin would take an L in his neuroscientific research of psychedelics. When assessing the capability of certain psychedelics on the brain, he assumed (1924, p. 8) that black people naturally had a higher recovery rate than whites:
“We may take it as a fact that Negroes have greater recuperation powers than white people. This is due not to climatic conditions but to certain innate qualities possessed by them.”
In his writings, he didn’t seek to prove this theory — it was just taken as matter-of-fact; another symptom of the 19th century. Lewin also insisted Indigenous people knew of their own racial inferiority, which is why they self-medicated with psychedelics:
“The Indians of South America are said to have an intuitive appreciation of their own defectiveness, and to be ever ready to rid themselves of such melancholy feelings by intense excitement, i.e. through kola and similar drugs” (p. 2).
Still somehow, Lewin believed psychedelics ‘form bonds in people of all walks of life’ (p. 7). He realized the diversity of people was so great that a one-size-fits-all explanation of human physiology and psychology in regards to psychedelics wouldn’t suffice. Likely influenced by Darwin’s The Origin of Species, Lewin made a strong case for the adaptations of organisms to a variety of external influences like psychedelics. He believed a skilled anthropologist could trace the development of culture directly to the availability of psychedelics, an idea shared 100 years later in Terence McKenna’s Food of the Gods. Lewin was also one of the first scientists to see the health benefits of psychedelics, mostly based on accounts of Indigenous people taking them for mental health.

In the 1800s, a small but prevailing idea amongst scientists was that psychedelics created a “trip” by activating ductless glands in the body to secrete hormones into the endocrine system. Lewin thought the theory was BS and instead theorized that psychedelics excite certain “brain centers” to “transmit agreeable sensations” (p. 3) through the chemistry of the substance. He basically described what we now know as psychedelics acting as serotonergic agonists that bind to mostly 5-HT2A receptors in the brain — an original theory Lewin established nearly 50 years before the discovery of serotonin.
Lewin’s assumption that psychedelics hit specific cortical regions through something like the serotonin system was remarkable, but only because he made other successful guesses like recognizing that every chemical study on the brain up to that point was conducted ex vivo, or on a dead brain, and that in vivo neuro research conducted on a living brain may have chemicals that were not present or didn’t transform into something else upon death. He also knew about the brain’s need for oxygenated blood and suggested that psychedelics may affect this process. Neuroscience had to wait 100 years for Lewin’s idea to be tested with BOLD (Blood Oxygen Level Dependent) brain imaging through MRI.
When it came to theoreticals, Lewin had a few. One of his notable ones was the idea of a toxic equation, which is a loose formula that dictates everyone has a certain resistance to the effects of psychedelics based on their neurophysiology and overall physiology. On the surface, it sounds like a reasonable idea, but digging deeper, it gets a bit irrational. His general belief was that people built up a resistance to psychedelics due to parts of the brain weakening and not being able to process these substances. There’s still no proof of this over a century later though, and in 2021, Dr. Ling-Xiao Shao conducted research that pointed to the opposite. Psilocybin actually strengthens dendritic density in the brain and repairs neurons that have atrophied due to stress and depression. Lewin also believed cells had ‘will-power’ and when a person takes a psychedelic after not taking it for a long time, the memory of the ‘agreeable sensation’ is just too strong to resist and that’s how people become addicted again (p. 18).
Unfortunately, psychedelic neuroscience research didn’t really catch on in the 19th century, mostly because civilization almost collapsed due to a global opioid addiction that crippled nearly every economy and led to prohibition in the early 1900s. The bigotry and racism of the 19th century confined Louis Lewin’s research of psychedelics into a box that takes a lot of ethical unpacking to fully absorb.
The origin of neuroscience is shrouded in poorly constructed science and whacky ideas which were specifically designed to marginalize groups of people from the discussion of who could be considered human. It has a dark past, but with a more defined scientific method and newer ideas, the future of psychedelic neuroscience is whatever we make it. In every natural system, diversity is the key defining factor for the progression of that system. These ideas aren’t mine or even new — Darwin wrote several books on this. This same need for diversity also applies to psychedelic neuroscientific research. History shouldn’t serve as an obstacle for the exponential amount of discovery that can be revealed if we all work together. We will get there.
This week’s Solidarity Fridays episode is another 2-parter: A Joe and Kyle discussion followed by the recording of Joe’s interview from Meet Delic with CEO of MINDCURE, Kelsey Ramsden.
In part 1, Joe and Kyle address a recent issue with the Facebook group and a rather accusatory tweet, then discuss something most people who are excited about the prospect of ketamine as medicine aren’t talking about: whether or not ketamine is addictive and therefore a concern for people with substance-abuse issues. And they talk about a Vice article showing some of the shortcomings of Mindbloom and how they highlight the various issues with at-home ketamine therapy and what really counts as ketamine therapy vs. just simply using ketamine. And lastly, inspired by PT writer Zeus Tipado‘s tweet, they wonder if “mystical” is the word we should be using to describe the psychedelic experience – and is the mystical what we should always be striving for?
And in part 2, recorded in a White Castle parking lot in Las Vegas, Joe briefly speaks with Kelsey Ramsden, CEO of MINDCURE. She discusses iSTRYM, their app designed to use A.I. to examine real-time data from users and provide drug-agnostic insights and recommendations, as well as collect and update different protocols for physicians to use with clients. And she talks about MINDCURE’s other big piece, the Desire Project, which is researching MDMA (and possibly other drugs) to help with Hypoactive Sexual Desire Disorder (HSDD), an affliction that leaves women unable to feel sexual desire (and is much more common than you may think). MINDCURE will also be manufacturing synthetic ibogaine for research studies.
“It is interesting when I hear people talk about psychedelics and always wanting to talk or be oriented towards the mystical. …Is it always mystical? Is that something that we always need to point towards for these experiences?” -Kyle
“When my undergrad was going on, I was kind of obsessed with this idea of enlightenment, opening up the chakra system, kundalini experience, etc., because I was positive that once I had that, everything else in my life was going to be solved. …I found an intellectual runaround to the suicide thing. It was a spiritual, intellectual solution to my deep dissatisfaction to how my day-to-day was looking. So I was really obsessed with transcendence and mysticism and all this other stuff as a way to avoid my life – classical spiritual bypass. And people may wonder why I have a little bit of snark around this topic. It’s because I lived it. I was there, I was in it. I was not doing very healthy stuff on the regular and also having this kind of interesting transcendent thing I was looking for that would ‘solve everything.’ And that’s what people are looking for, is a single thing to solve their lives and then everything’s good from there. Well, no. You’re not going to get that.” -Joe
From Kelsey Ramsden’s segment:
“I think the sleeper (the secret sauce, if you will) is the protocol catalogue: this idea that a therapist can unlock a variety of protocols in there for different patients and get personalized care at that level, as well as it lets all of us who are developing protocols and drugs get a new revenue line. …We have the content and we distribute it and so that allows us to pick up value at every segment of the value chain, and create an amazing product that can unify mental health care globally. That’s a big statement, but there’s no reason we can’t.”
“I think data’s going to move the science. We know that and that’s what we’re all working on. But story is going to move the culture. I was on a panel the other day and someone was smacking down one of the people who has enrolled a celebrity spokesperson. But for a segment of the population, we’re still in an echo chamber. We’re still in our small world. [Celebrities can move the needle] if it’s the right person with the right message at the right time, for the right audience. …If the right people can put their hand up and say ‘I did this, it helped me, it changed my life,’ and that makes someone explore it and make their own opinions? Amazing. There was someone like that for me.”
From Joe and Kyle’s segment:
@therealbrom’s twitter thread about ketamine and addiction
Vice.com: Psychedelic Telemedicine Has Arrived. What Could Possibly Go Wrong?
Psychedelics Today: Dylan Beynon – Mindbloom: The Next Chapter in Mental Health and Wellbeing
Zeus Tipado’s twitter thread about mysticism
Snowboarding to Nirvana: A Spiritual Journey, by Frederick Lenz
From Kelsey Ramsden’s segment:
Mindcure.com: Mind Cure Promotes Kelsey Ramsden to President and Chief Executive Officer
Vicetv.com: Hamilton’s Pharmacopeia: Synthetic Ibogaine — Natural Tramadol
Mindcure.com: MINDCURE Provides Update on Studies and Clinical Trials
Stylist.co.uk: When Harry Met Sally’s iconic orgasm scene almost didn’t happen
 With Over 15 years founding, scaling, and operating innovative businesses across several industries, Kelsey Ramsden has built multiple eight-figure companies from the ground up. She is an experienced leader and acclaimed entrepreneur, twice recognized as Canada’s Top Female Entrepreneur of the Year. After serving as MINDCURE‘s COO, Mrs. Ramsden steps into the President and CEO role as of December 1, 2020. She possesses a thorough understanding of the mental health industry and a clear vision of where it is going.
With Over 15 years founding, scaling, and operating innovative businesses across several industries, Kelsey Ramsden has built multiple eight-figure companies from the ground up. She is an experienced leader and acclaimed entrepreneur, twice recognized as Canada’s Top Female Entrepreneur of the Year. After serving as MINDCURE‘s COO, Mrs. Ramsden steps into the President and CEO role as of December 1, 2020. She possesses a thorough understanding of the mental health industry and a clear vision of where it is going.


