Could a nation defined by inflammation find relief in psychedelics?
It’s a verifiable truth that the United States of America may be considered a global leader, especially when it comes to the prevalence of mental and physical health disorders. In fact, of the nearly 330 million people in the population, millions to hundreds of millions of Americans suffer from chronic conditions like:
- Obesity (42%)
- Arthritis (24%)
- Anxiety (19%)
- Irritable Bowel Syndrome (IBS) (15%)
- Allergies (15%)
- Attention Deficit Hyperactivity Disorder (ADHD) (14%)
- Diabetes (11%)
- Depression (8%)
- Asthma (8%)
- Cancer (6%)
- Autism (2%)
- Fibromyalgia (2%)
These sobering statistics beg the questions: How could a single nation of relatively modest size be home to such a vast selection of chronic diseases? And how could psychedelics be used to combat these conditions affecting so much of the population?
Why is Inflammation so Prevalent?
The answer begins with key lifestyle factors such as diet, exercise, tobacco use, or genetic predispositions, each of which contribute to the pathology of a given disease. For example, a 2010 study by the American Cancer Association found that 90% of Americans don’t meet their daily recommended requirement of vegetables, with 75% failing to eat even a single piece of fruit during an average day.
The American diet overall is egregiously devoid of whole grains, beans, fruits, vegetables, and nuts, with the US Department of Agriculture estimating they represent a mere 11% of the populous’ typical daily food intake. Despite this lack of prevalence, these unprocessed natural foods are otherwise rich in medicinal phytochemicals found to support the immune system and strengthen the body’s resistance to infections, as well as fight cancer and diabetes; diseases that are twice as prevalent in the US relative to the global average. Shockingly, the US also leads the world in obesity rates by nearly 400%, and is first in global consumption of sugar, outranking Germany by about 26% yearly.

Although diet quality is proven to significantly impact the likelihood of disease development, what Americans eat is only one contributing factor among many. Poor diet alone doesn’t explain the exceptional amount of chronic health conditions seen in the population. In fact, it’s estimated that over 60% of Americans suffer from at least one chronic health condition, 42% of the population are diagnosed with at least two, and up to 12% of Americans live with five or more chronic diseases.
To put those percentages in perspective, the 2020 election saw the highest voter turnout in 120 years, with the most votes for a single presidential candidate ever recorded in American history. Joe Biden reportedly received over 81 million popular votes, representing less than half of the 198 million Americans suffering from at least one chronic health condition, and only marginally more than half of the 139 million with at least two.
Despite the fact that they’re by no means a minority in the population, chronic diseases are found to disproportionately affect socioeconomic minorities in the United States of America and beyond. A recent study published in the journal, “Archives of Public Health,” used 20 years (1995-2015) of empirical data from the Organization for Economic Cooperation and Development (OECD) to investigate the impact of education on health across the populations of 26 countries, including the United States, Canada, United Kingdom, France, Germany, and other founding nations that became members when OECD was created in 1960. This data, taken from millions of people in numerous countries across the globe over one fifth of a century, clearly demonstrated that higher educational attainment in adults positively correlates with longer lifespans, better health outcomes, increased Gross Domestic Product (GDP) per capita, and reduced infant mortality rates.
Put simply, the OECD data suggests that highly educated adults with ample finances generally live up to 12% longer (8-10 years), enjoy healthier lives, make more money, and are less likely to die at birth or of cancer, when directly compared to individuals of lower socioeconomic status (SES). Unsurprisingly, adults with higher GDP per capita also spent more money on healthcare and education over their lifetime, with college and university education found to positively influence life expectancy, child vaccination, and enrollment of children in education, as well as negatively impact infant mortality. Taken as a whole, the OECD data demonstrates an essential principle:
If appropriate education and adequate income significantly increase life expectancy, then access to quality schooling, sustainable employment, and equitable socioeconomic mobility are inherent to health care services.
However, even if we factor in education and employment as essential contributors to health, the fact remains that as of 2021, over 85 million Americans older than 25 had attained a Bachelor’s Degree or higher, and US unemployment was a mere 3.7% in August 2022. Since neither education nor employment are able to fully reconcile the disproportionately large number of Americans currently suffering from chronic health conditions, there must be a deeper underlying cause contributing to the pathology of diseases reportedly observed in the country’s citizens and resident aliens.
What is Chronic Inflammation?
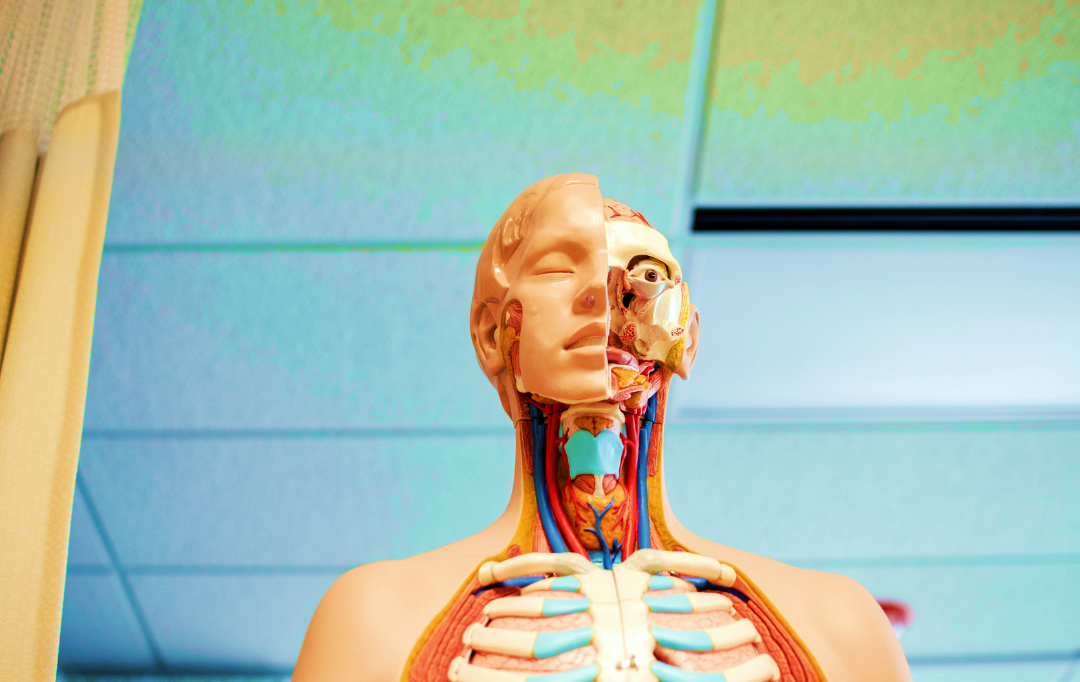
Compellingly, inflammation has been identified as a central contributor to all aforementioned chronic health conditions and beyond, and is implicated in over 60% of all human deaths around the globe. Some may already be familiar with acute inflammation in the form of localized pain, redness and swelling, usually in response to an injury or infection. Acute inflammation is typically a normal immune response during which the immune system is activated through the release of specific proteins, essentially called inflammatory markers. These markers then act as beacons to recruit immune cells, which subsequently migrate to the particular body part(s) in need of defense or repair.
In contrast, chronic inflammation is less apparent and far less immediate, but has insidiously dire consequences when left unchecked. Instead of causing localized pain or swelling, chronic inflammation causes systemic issues with immune cell signaling through excess “noise” created by high levels of inflammatory markers. Rather than being recruited to areas of the body most in need of healing, immune cells are drowned in an overwhelming number of biochemical beacons and ultimately disoriented. By disrupting this essential communication between immune cells, chronic inflammation prevents the appropriate direction of immune cells to critical issues needing attention, and may instead direct disproportionate amounts of immune activity to arbitrary areas – thus crippling the body’s capacity to effectively heal itself or prevent systemic disease.
The dysregulation of the immune system may ultimately induce the development of one or a combination of diseases, including autoimmune disorders like Crohn’s Disease, IBS, Alzheimer’s, arthritis, and diabetes, as well as various cancers and neurological disorders. Furthermore, children of mothers with chronic inflammatory conditions are demonstratively more likely to be diagnosed with ADHD, anxiety, depression, obsessive compulsive disorder (OCD) and autism, especially when chronic prenatal exposure to maternal inflammatory markers is exacerbated by psychological or physiological stress.
Over the past 20 years, a growing body of research has further investigated the complex relationship between chronic inflammation, various mental and physical diseases, and socioeconomic status (SES). High levels of inflammation measured by markers in the blood of low SES patients were found to prospectively predict whether they would suffer from depression, heart disease, ischemic stroke, and/or mortality.
Furthermore, factors such as poverty, lack of social or educational resources, obesity, and diets rich in refined sugar were all closely associated with increased inflammatory markers, chronic diseases, and mortality rates. Stress derived from socio-political, financial, environmental (chemical, biological, electromagnetic), or psychosocial (relationship experiences, trauma, social conditioning) aspects of a patient’s life also reportedly influenced inflammation, with chronic psychological and emotional stress inducing a significant increase in observed blood inflammatory markers; thus promoting immune dysfunction and ultimately increasing the likelihood of chronic diseases in individuals of low SES.
Psychedelics as Anti-inflammatory Medicine
Despite these undeniable correlations and profound implications, the medical model of inflammation as the root of disease is not a new concept. Whether willow bark or aspirin, both traditional Ayurvedic and modern Western medicine employ preparations of anti-inflammatory drugs to treat a number of maladies, from headaches to heart disease. In fact, many over-the-counter (OTC) medications, commonly prescribed pharmaceuticals, and even psychedelic drugs owe some portion of their medicinal benefits to anti-inflammatory effects exerted in particular tissues of the human body.
For example, recent research has revealed that two of the most commonly prescribed classes of antidepressants, Selective Serotonin Reuptake Inhibitors (SSRIs) and Selective Norepinephrine Reuptake Inhibitors (SNRIs), may instead induce their expected medical effect via anti-inflammatory action within the brain itself, thus alleviating underlying neuroinflammation implicated as a central contributor to malaise, fatigue, brain fog, emotional reactivity, and other psychological symptoms. This revelation casts significant doubt on the broadly accepted model for the pathology of depression that classically purports serotonin deficiency as the primary cause. Today, a new breed of antidepressants specifically intended as anti-inflammatory drugs are undergoing feverish development by major drug corporations.
But before we herald these pharmaceutical innovations as the ultimate solution to tame the treachery of chronic neuroinflammatory disease, we must address the unjust marginalization and criminal victimization of disaffected Americans self-medicating via naturopathic means. Notwithstanding their evolutionary, anthropological, and social significance, the potent anti-inflammatory effects of cannabis, psilocybin mushrooms, and other psychedelic derivatives are now well-supported by an ever-growing body of recent scientific research. Although prohibitionist laws previously precluded a thorough investigation of their potential, the US has slowly and begrudgingly allowed the pursuit of psychedelic pharmacological power. As the barriers of outdated, impermissible, and fallacious legislative paradigms fall, clinicians are finally gaining critical insights that have enabled the development of novel pharmaceutical psychedelic derivatives with extreme precision; such that specific medical characteristics like an anti-inflammatory effect or psychedelic effect may be intentionally targeted and enhanced or diminished.

However new this scientific perspective may seem, medicinal preparations of psychedelics have reportedly been used for centuries, and even pharmaceuticals investigated and approved for clinical use decades ago were arguably directly modeled after psychedelics like LSD and psilocybin. Most notable of these compounds, Methergine (methylergometrine), is an LSD derivative used to induce contractions during childbirth since 1582, and is currently included on the World Health Organization’s (WHO) List of Essential Medicines. A similarly indispensable class of pharmaceutical psychedelic derivatives, the triptans, were first developed and patented in 1991 to treat migraines and cluster headaches, conditions which are both implicated to be caused by neuroinflammation. Interestingly, early triptans display remarkable structural similarities to tryptamine psychedelics like DMT and psilocybin.
Further progress spearheaded by brave and dutiful psychonauts in professional practice, underground social circles, and beyond has steadily illuminated the psychological and pharmacological nuances of many psychedelic drugs, revealing that they’re in fact highly safe and effective treatments for Post-Traumatic Stress Disorder (PTSD), suicidality, depression, anxiety, addiction, Fibromyalgia, various chronic inflammatory diseases, and more. Tireless efforts across decades of clinical trials using psychedelics such as cannabinoids, MDMA, ketamine, and psilocybin have paved the way to their current or imminent approval by the US Food and Drug Administration (FDA).
It finally seems quite possible that psychedelic medicines previously incorrectly admonished as “psychomimetic drugs” that imitated psychosis, damaged DNA, and were toxic to the human body may soon be available as legitimate pharmaceutical compounds aiming to alleviate the suffering of millions. With the current medical and legal trajectories, it’s highly likely that sometime in the not-so-distant future, inflamed Americans in need of psychedelic therapies will be able to access them without the unnecessarily harmful (but now still-looming) threat of social, criminal, and civil persecution. As much as one author celebrates this opportunity for a modicum of much needed progress in the United States, a single question remains:
Do a handful of state-level decriminalization initiatives for some select drugs, as well as the monetization and regulation of a limited number of pharmaceutical psychedelics at the federal level truly represent a sufficiently compassionate and broad solution to remedy the innumerable and egregious offenses against American life, liberty, and the pursuit of happiness committed by the war on drugs?